Alumni and Friends
Support Harvard Chan School
Philanthropy powers research and education
New federal policies are profoundly disrupting the decades-old partnership between the U.S. government and research institutions like Harvard Chan School. These policies threaten to severely restrict federal research funding for scientists working on public health, creating an unprecedented financial crisis for our School.
As we navigate these challenges, philanthropy is essential to powering our research and educational programs. Harvard Chan School needs your support to continue our mission: improving health and advancing equity so all people can thrive.
Our alumni and friends provide critical resources to educate the next generation of public health leaders; empower faculty to pursue groundbreaking research; and translate those insights into real-world solutions to global health challenges.
Living Proof that Our Mission Changes Lives
Harvard Chan alumni are the hope of our school realized. Read about some of the thousands of our alumni who are creating waves of change across continents and generations.



Annual Giving
We hope every member of our community makes a gift each year. Unrestricted gifts of any size provide leadership with the flexibility to put resources where they are needed most. This agility allows us to seize opportunities, respond swiftly to challenges, and support every area of the School’s work while advancing health and dignity for all.
Support Students
Your gift to financial aid supports exceptional students—60% of whom rely on financial aid to attend.

Support Faculty
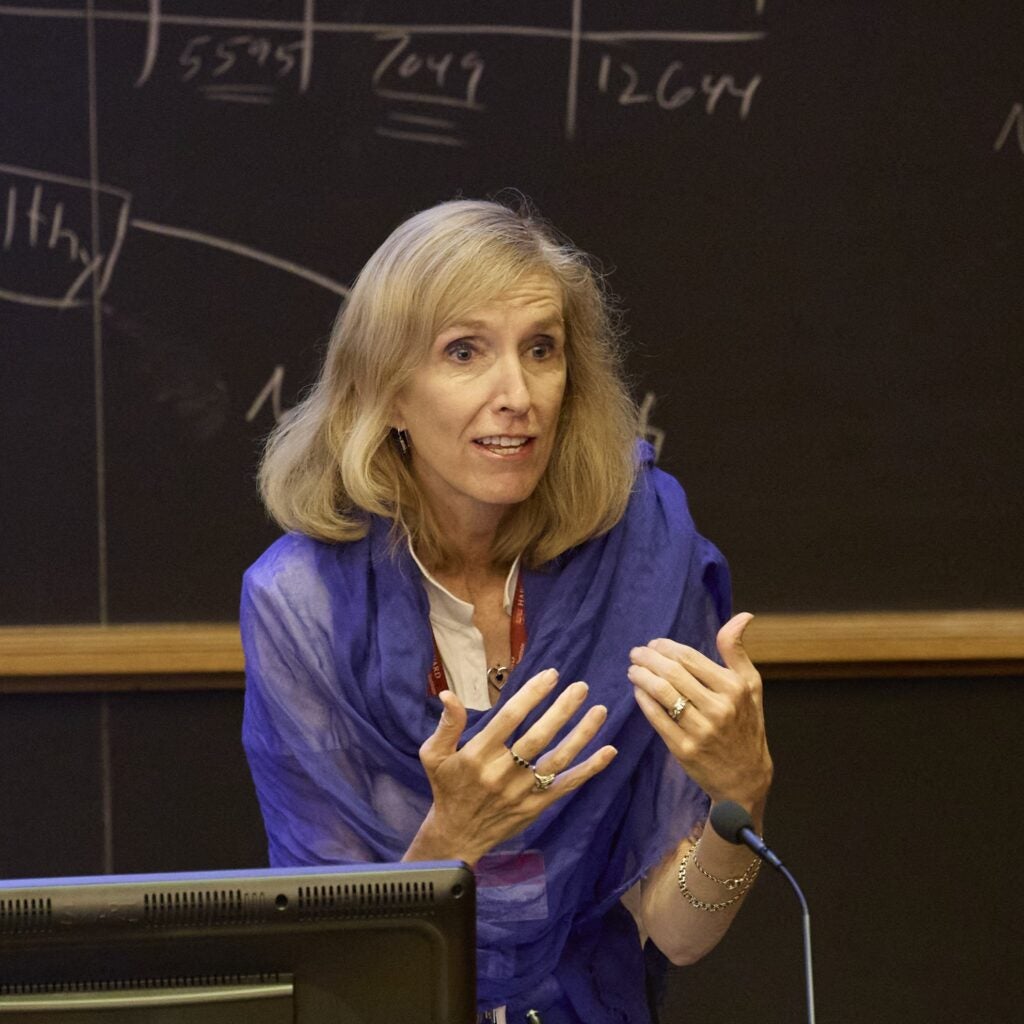
Faculty shape the future of public health through critical research and teaching.
Support Research
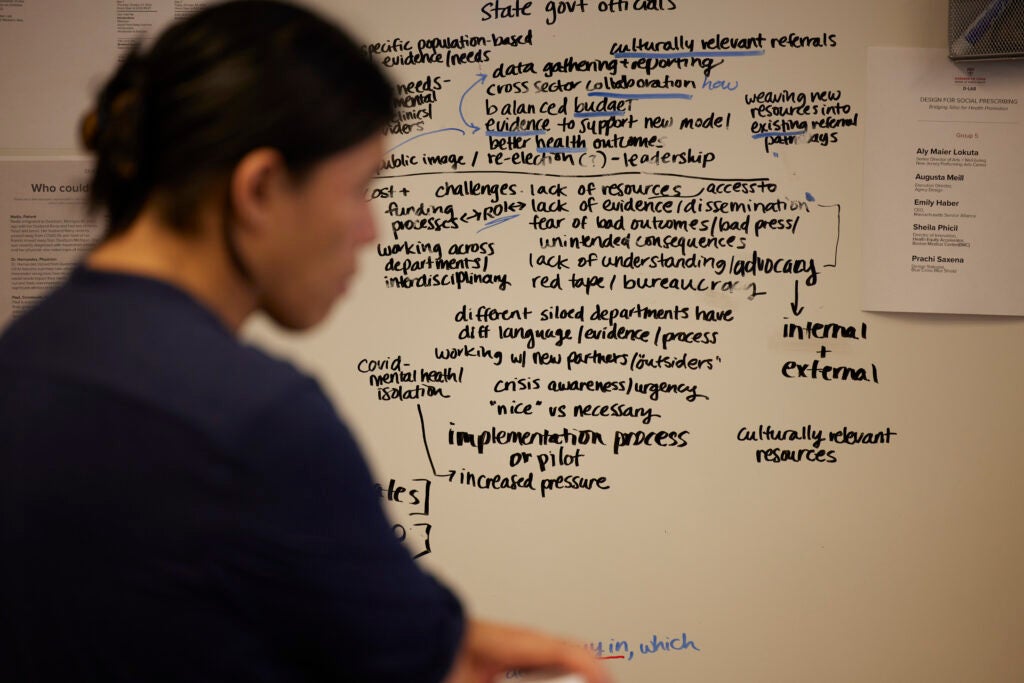
Researchers’ groundbreaking ideas catalyze real-world solutions.
Dean’s Leadership Fund
This fund empowers Harvard Chan School to seize emerging opportunities and tackle complex challenges with agility and vision. Providing maximum flexibility for strategic investments in both education and research, this fund enables our leadership to advance bold initiatives that amplify our excellence and deepen our real-world impact. As we build toward a more focused and resilient future, the Dean’s Leadership Fund ensures we can act decisively to strengthen our position as a world-leading school—supporting breakthrough discoveries, expanding educational innovation, and forging powerful partnerships that create lasting change for global health.
Your Giving Drives Public Health Progress
Create Your Legacy at Harvard Chan School
When you make a major gift to Harvard Chan School, we can recognize your generosity by connecting your name—or that of a loved one—directly to our mission to improve health and promote equity so everyone can thrive. Your investment in our mission will create lasting change while we ensure your legacy lives on through every graduate who works to build a healthier world.


