High fruit and vegetable consumption may reduce breast cancer risk
 Women who eat high amounts of fruits and vegetables each day may have a lower risk of breast cancer, especially of aggressive tumors, than those who eat lower amounts, according to recent Harvard Chan School research. Cruciferous vegetables such as broccoli, and yellow and orange vegetables, had a particularly significant association with lower breast cancer risk.
Women who eat high amounts of fruits and vegetables each day may have a lower risk of breast cancer, especially of aggressive tumors, than those who eat lower amounts, according to recent Harvard Chan School research. Cruciferous vegetables such as broccoli, and yellow and orange vegetables, had a particularly significant association with lower breast cancer risk.
The investigators analyzed diet questionnaires submitted every four years by participants in the Nurses’ Health Study (88,301 women, starting in 1980) and the Nurses’ Health Study II (93,844 women, starting in 1991). Women who ate more than 5.5 servings of fruits and vegetables each day had an 11 percent lower risk of breast cancer than those who ate 2.5 or fewer servings. Higher consumption of fruits and vegetables was particularly associated with lower risk of more aggressive tumors, including ER-negative, HER2-enriched, and basal-like tumors.
Previous work by the research group linked reduced breast cancer risk to higher fiber intake, but the benefits of cruciferous vegetables, as well as fruits and vegetables rich in beta-carotene, found in the new study appear to be independent of their fiber content, says first author Maryam Farvid, research scientist in the Department of Nutrition. This suggests that constituents of these foods, such as antioxidants and other micronutrients, may themselves be important in reducing breast cancer risk. Read more

Alice Hamilton sculpture unveiled
The School unveiled a bust of Alice Hamilton, Harvard’s first female faculty member, on September 26 in the François-Xavier Bagnoud building lobby. In remarks during the unveiling ceremony, Dean Michelle A. Williams said the statue would remind women and men of Hamilton’s accomplishments and her breaking of centuries-old barriers. Hamilton, who was appointed assistant professor of industrial medicine in 1919, was a leading authority on workplace health. She conducted pioneering studies on the toxic effects of lead and mercury exposure in manufacturing—research that contributed to government reforms to improve the health of workers. Hamilton’s appointment was subject to three restrictions: She was not allowed inside the Faculty Club, she could not participate in processions at commencement, and she was not eligible for faculty tickets to football games. Read more
“Behavioral nudge” influences doctors’ prescribing habits
Sending doctors letters informing them that they are high prescribers of a potentially dangerous medication and under scrutiny from Medicare is enough to lead them to write fewer of those prescriptions, according to a study from researchers at the Harvard Chan School and Columbia University’s Mailman School of Public Health. The study targeted 5,055 primary care physicians nationwide who were the most frequent prescribers to Medicare patients of Seroquel (quetiapine)—an antipsychotic with potentially harmful side effects in the elderly. Half of the doctors received letters stating that their quetiapine prescribing was high relative to that of their peers and was under review. The other half of the group received letters about an unrelated Medicare regulation.
Physicians who received the peer-comparison letters cut their overall quetiapine prescribing for Medicare patients by 11 percent over the subsequent nine months and 16 percent over the subsequent two years. New prescriptions of the drug dropped by 24 percent over two years. “Overprescribing of antipsychotic drugs is a huge and persistent problem, particularly in the elderly,” notes Michael Barnett, assistant professor of health policy and management at the Harvard Chan School and second author on the study. “These results are striking for an intervention as simple and cheap as sending letters.” Read more
Boxers or briefs? Loose-fitting underwear may benefit sperm production
 Men who most frequently wore boxer shorts had significantly higher sperm concentrations and total sperm counts than men who wore other types of underwear, according to research led by the Harvard Chan School. The findings of the study, which collected information and semen samples from 656 men at the Fertility Center at Massachusetts General Hospital, suggest that certain styles of men’s underwear may alter sperm production. “These results point to a relatively easy change that men can make when they and their partners are seeking to become pregnant,” says Lidia Mínguez-Alarcón, lead author and research scientist in the Department of Environmental Health.
Men who most frequently wore boxer shorts had significantly higher sperm concentrations and total sperm counts than men who wore other types of underwear, according to research led by the Harvard Chan School. The findings of the study, which collected information and semen samples from 656 men at the Fertility Center at Massachusetts General Hospital, suggest that certain styles of men’s underwear may alter sperm production. “These results point to a relatively easy change that men can make when they and their partners are seeking to become pregnant,” says Lidia Mínguez-Alarcón, lead author and research scientist in the Department of Environmental Health.
Among the study participants, 53 percent reported usually wearing boxers. Analysis of semen samples showed that these men had 25 percent higher sperm concentrations and 17 percent higher total sperm counts, compared with men who did not primarily wear boxers. Men who wore boxers also had higher percentages of motile sperm, which can move through the female reproductive system and fertilize an egg. Read more
Harvard Chan researcher helps shape new cervical cancer screening guidelines
New guidelines for cervical cancer screening—based in part on research by the Harvard Chan School’s Jane Kim, professor of health decision science in the Department of Health Policy and Management—were published in August 2018 by the U.S. Preventive Services Task Force (USPSTF). The USPSTF commissioned Kim’s team to analyze various screening scenarios using mathematical modeling. The investigators looked at 19 different screening options, such as Pap testing alone, HPV testing alone, and Pap and HPV “co-testing,” and considered different starting ages and different screening intervals. They also considered which options would provide the biggest health benefit to women (such as fewer cervical cancer–related deaths) as well as which would cause the most harm (such as additional and perhaps unnecessary invasive tests). The USPSTF’s 2012 cervical cancer screening guidelines had recommended that women get Pap tests every three years from ages 21 to 65, with an option to switch to co-testing every five years at age 30. Kim’s modeling showed that, compared with the 2012 recommendations, certain strategies using HPV testing alone could lead to near-equivalent or better health benefits. Read more
Could a nanofiber help fight obesity?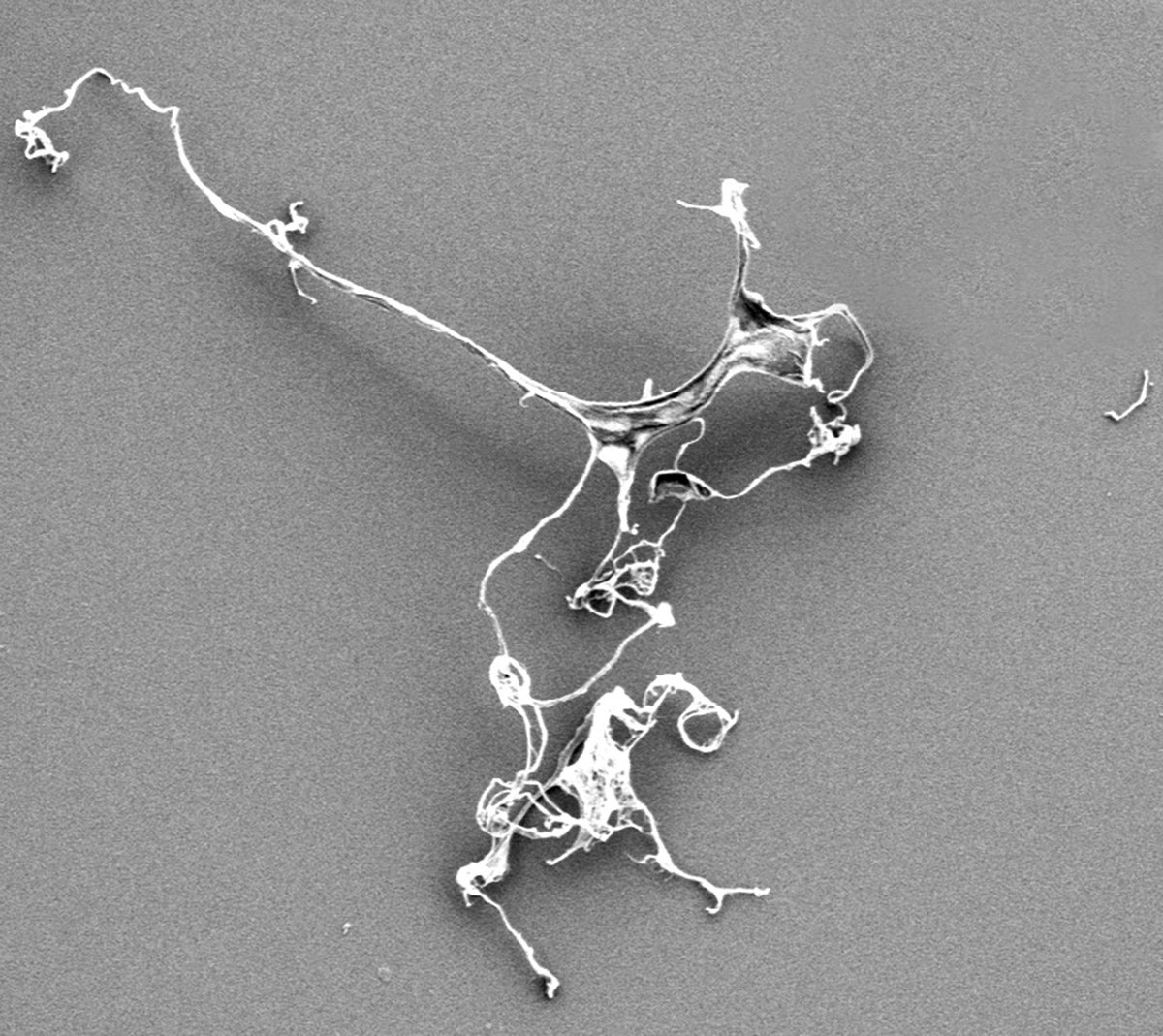
You won’t smell it. You won’t taste it. And you certainly won’t see it. But a nanocellulose material derived from all-natural substances could potentially become a food additive that reduces fat digestion and absorption and aids in weight loss.
Researchers at the Harvard Chan School discovered that when cellulose—a natural biopolymer—is engineered into “spaghetti-looking fibers” a mere 50 nanometers in diameter, it can stop fat from being digested. In a recent study, rats that were fed heavy cream containing nanocellulose absorbed 36 percent less fat than rats fed regular heavy cream.
“It’s like having your cake and eating it too,” says Philip Demokritou, senior author of the study and director of the School’s Center for Nanotechnology and Nanotoxicology. “And there are no chemicals. I believe that we should learn from nature and use more nature-inspired and derived materials. There’s 4 billion years of free R&D there.” Read more
– Madeline Drexler is editor of Harvard Public Health.
Photos: Tom Hill/Alamy, Nilagia McCoy/Harvard Chan School, iStock, Rusian Kudrin/Alamy, Center for Nanotechnology and Nanotoxicology







