INTERVIEWS AND TEXT
Madeline Drexler, Editor, Harvard Public Health
PHOTOGRAPHY
Kent Dayton
ISSUE
Fall 2020
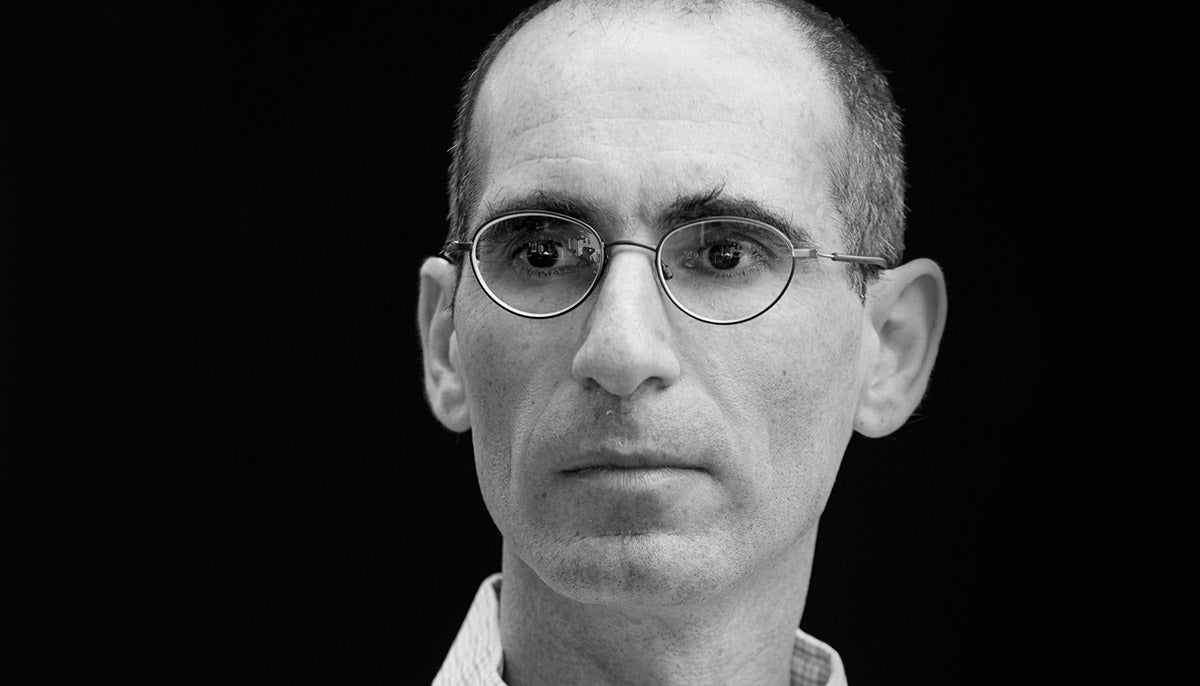
Truth Teller

Marc Lipsitch
Professor of Epidemiology
Founder and Director, Center for Communicable Disease Dynamics
When did I realize this could be serious? I remember very distinctly. On January 21 and 22, I was in an NIH [National Institutes of Health] meeting in Maryland about biosecurity and the risk of laboratory accidents—issues I’ve been working on for a few years. There were a lot of flu virologists and coronavirologists there. They were saying: Could this be the big one? I came back from that meeting hoping it wasn’t the big one, because I wanted to get on with my other work, but I was certainly attuned.
Was I scared? Not yet. I try hard to distinguish what’s known to be true from what’s possibly true from what’s definitely not true from what’s opinion. That’s how you should think when you’re being analytical. And I’m actually pretty good at being analytical—until I’m not. [Laughs.]
In late January, I was still pretty analytical, in part because the outbreak was so far away physically and felt far away temporally. My thinking was, “Here is something that’s happening that we should respond to because it’s what we do.” Rather than, “Oh my God, life is going to get really bad for the foreseeable future.” That came later.
•••
In February, I was watching the prime minister of Singapore’s video on Facebook. He said, very calmly, “We’ve been through this before. There’s something new happening. We’re going to do our best to control it. We probably will fail. But we are better prepared than we’ve ever been, and this is how we’re going to deal with it.” I thought, “Wow, that’s an admirable message to give your country. Wish we had something like that.”
Truth telling is important, but even more important, perhaps, is having a strategy that’s coherent and comprehensive. What’s been missing in the U.S. is a strategy. There hasn’t been one. The pandemic is a problem of public health, a problem of industrial policy, a problem of hospital health care systems, a problem of economics, of education, of social welfare, of mental health. A functioning nation would see that pretty early on and devote strategic thinking to how to deal with it on all those fronts. Instead, we just messed around. It is hard to think of a crisis for which this administration is more unsuited, in the sense that you need strategy, subtlety, consistent truth telling.
I suspected from the start that there would be a lack of clear communication from the federal government. So I made a very conscious decision that, if the government is not going to be a source of reliable information, then we as a scientific community will have to step in. My Twitter followers have gone from about 4,000 in early January to about 206,000 today. I think plain talking, admitting what’s known and what’s not known, gets you a long way, at least with thoughtful people.
For example, I hate wearing a mask. [Laughs.] It’s gross to wear a mask all the time. But admitting it is better than saying, “We must wear masks. It’s good to wear masks. You should enjoy wearing a mask.” That’s just false. Somebody said that they found it very helpful that I admitted how much I hate wearing a mask.
When I’m arguing in favor of an intervention—like wearing a mask or social distancing—I try to point out that it’s not that it’s an unrestricted good and the alternative is an unrestricted bad. All these control measures have huge costs. Denying that is both dishonest and makes people not trust you. If you say this is going to be really awful but the alternative is more awful, that’s much more reasonable in this kind of situation than to say we must do X and it will go fine.
What do I tell policymakers? One theme is just the very simple point that the virus doesn’t have an inherent tendency to go away. It has an inherent tendency to spread in proportion to how many contacts we have. If we dial up the contacts, we’ll have more spread. If we dial down the contacts, we’ll have less. Putting aside the debate about whether a virus is alive or not, it’s an entity that has its own rules. Wishful thinking is not a productive approach.
•••
Almost the first thing we did, as a research-cum-public-health-practice activity, was a little simulation of introductions of cases into the country and the potential consequences. It was in February, very early on. It was done initially because somebody in the New York City Health Department asked us to do it.
Back then, all of the parameters were uncertain. The reproduction number is still uncertain, but it was really uncertain then. The proportion of asymptomatic transmission was uncertain, and still is. We made a little web app that played out various scenarios. In some of the scenarios, the epidemic takes off. In others, it doesn’t. In some, there are very few cases by April. In others, there are thousands or tens of thousands of cases by April.
At the time, I thought, “They’ve asked us to do it, we’ll do it. But I don’t understand what the purpose is. Obviously, the outcomes are uncertain, and you should be preparing as if there could be cases that you don’t know about yet.” The simulation was a pure expression of uncertainty, because even if you fix all the parameters, you don’t know what’s going to happen. If you vary them, it becomes even more uncertain because of random effects—sometimes epidemics die out, sometimes they don’t.
What happened, based on what I’ve heard from reporters who dug into this, is that the simulation made a huge difference to planners in New York City. What it conveyed was that absence of evidence is not evidence of absence. We don’t know if there will be zero cases or 100,000 cases in late April. That means that you don’t know either, so you should plan to try to prevent the latter. Putting it in mathematical terms in a simulation where you could twiddle the knobs apparently made it real for people in a way that just saying it did not. It may have been one of the best things we’ve done in this pandemic.
•••
The last time I communicated with the White House was March 26. I spoke to Deborah Birx’s assistant. [Deborah Birx is the White House coronavirus response coordinator.] At that time, there were about 1,300 deaths and 85,000 cases in the U.S. [Editor’s note: As of September 30, there have been some 200,000 deaths and 7 million confirmed cases.]
You know, it’s not about me. I don’t feel an entitlement to be in communication with the White House. But I do feel an entitlement, as a citizen, to have the White House use good science. The fact is that they are not using science to improve the response as much as they should. They’re often using bad science to make the response worse. It’s so frustrating, so unnecessary. It’s a self-inflicted wound.
explicator

Ashish Jha
Former Director, Harvard Global Health Institute
Former K.T. Li Professor of Global Health
Dean, Brown University School of Public Health
Talk about getting things wrong. In January, when I started hearing about the virus in China, I basically said that I worried a lot about the global response and the WHO [World Health Organization] and American global leadership. But—and I said this quite explicitly—I didn’t worry about America and the American response, because we had the CDC [U.S. Centers for Disease Control and Prevention], and the CDC is the best public health agency in the world.
At the time, I was on sabbatical in Europe. Over February, as I was watching the world respond, I had this gnawing feeling that things were not developing the way they should be in the U.S. My sense was that we didn’t have a testing infrastructure up and running.
I returned home on March 3 or 4. All of a sudden, I realized how bad things were. We were seeing an uptick in cases in New York. We were starting to see community transmission. It dawned on me that the U.S. had wasted an entire six, seven weeks. I had underestimated our national ability to mess up this response. I didn’t think we could possibly get it this wrong.
•••
Fundamentally, we have an executive branch that has not wanted to try to solve this problem. Why did the Trump administration decide that they didn’t want to put in the work necessary to fight the pandemic? I don’t know. That is probably the most important question.
I’ve gotten calls from the White House, and in the various conversations I’ve had with people there, I’ve been very clear about what is necessary. I often say things that contradict what comes out of the White House. My general approach is to lay out the science as I understand it and ask them what I’m doing wrong, why my conclusions might differ from theirs. In every conversation that I have had—every single time, with no exceptions—the person on the other line has agreed with what I’m saying.
In fact, ironically, a couple of times, when I have said, “We need a lot more testing than you guys think we do” and walked through my logic, they’ve replied, “Actually, we probably even need more than that.” My response is, “Then why are you not just being honest with the American people, and why are you not working toward getting people what they need and what America needs?” The general response—these are the science people—is they can’t convince the political staff at the White House that they ought to be doing this.
Those science people are people you’ve heard of. People you’ve seen on TV. I would not put Tony Fauci [Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases] in this group, because Tony has been nothing but completely crystal clear.
I have gone from frustration to despondency to, at times, downright anger. One time, one of these people in the White House basically said to me, “Well, of course you are right, but there’s nothing I can do about it.” I was like, “So why are you there?” The person said, “If I left, the next person would be even worse.” I said, “How could they possibly be worse? You mean even less effective? Because you are being completely ineffective.”
•••
I was born in Bihar, a state in eastern India. My family moved to Canada when I was 8 and then to New Jersey. When I was in college, at Columbia, I had this sense of, “Am I Indian? Am I American?” It felt like this awful struggle, because I didn’t feel like I could possibly ever choose. First and foremost, I believe that there is a lot more in common among all of us than there is that differentiates us. The stuff that makes us human and makes us similar far outstrips what makes us different. That has been a shaping force in how I see the world.
I’m probably doing 10 percent of the media requests that I’m getting. I’m doing 15 to 20 media hits a day. My days begin around 5 or 5:15 in the morning and finish close to midnight.
Probably one to three times a day I get an email or a message through Twitter or direct messages or occasionally a text message, meaning somebody has my phone number—vitriolic, often racist. Pretty standard stuff. “Go back to where you came from.” “You’re not a real American.” Blah, blah, blah. On Twitter, after one of my TV appearances, someone wrote, “You’re nothing but a third-rate, Third World hack.” I thought, “Did you have to say that I’m an idiot and be racist?” One personal way I’ve changed as a result of this pandemic is that I’ve gotten a much thicker skin. Part of it is just desensitization. It’s unfortunate, right? Because racism is not something that we want to get desensitized to.
•••
This has been a catastrophic failure of leadership, in a way that is almost unimaginable. We happened to have leadership that decided that they were going to bluff their way through a pandemic. At every step, they minimized. At every step, they discounted. At every step, they tried to act like it wasn’t here.
At first, I kept thinking, “It can’t be this bad. There are going to be adults in the room. Someone’s going to step up. We’re going to get this right.” But every time I have thought it can’t possibly get worse, it has gotten worse.
Data Tracker/
Troublemaker

Caroline Buckee
Associate Professor of Epidemiology
Associate Director, Center for Communicable Disease Dynamics
Founder, COVID-19 Mobility Data Network
In epidemiological modeling, the important thing is being able to ask the right question. It’s understanding the biology deeply enough to be able to simplify it and formalize it in the language of math. You also have to understand reality. You have to understand the reality on the ground of what it means to collect data, where the data’s coming from. You have to understand the human structures that generate data. You have to understand what people need.
My focus has always been the very poorest, most vulnerable populations. I have worked on projects in Bangladesh, Colombia, Guyana, Kenya, Pakistan, and Thailand. My mobility data research originated because I was interested in migration and the geography of infectious disease, how it spreads.
In March, my colleagues and I began analyzing anonymized mobile phone data, both in the U.S. and abroad. Our question was: Can we find useful proxies for COVID-19 transmission, since we can’t see infections happening in real time, and we only catch up with them when somebody gets tested or hospitalized? Can we use mobility data to complement a surveillance system and give us an early warning of where we think transmission’s going to happen?
I think the answer is yes. That’s been clear, and we’ve been providing that kind of information to policymakers at the city level, at the state level, and internationally every day, for months.
•••
One thing I’ve learned in this pandemic is that we have consistently taken responses from Western and high-income countries and assumed that they could be applied to low- and middle-income countries. For example, stringent lockdowns or the idea that you could scale up PCR [polymerase chain reaction], or molecular, testing—those things are simply not possible in the places I have worked.
Let’s think about Guyana. In Guyana, you have remote Amazonian communities that can only be reached by a small plane and a boat. PCR testing only happens in the capital, because that’s where the lab capacity is. If somebody in a remote community comes into a local health clinic with a fever and a cough, even if a nasal swab test is available, you have to get that swab onto a plane that may fly only every other day to the capital. Then somebody has to run the PCR. Eventually, you get a result. But by the time you get that result back to the patient in the remote region, it’s irrelevant.
Or take the Rohingya refugee camp in Bangladesh. What does it mean for a refugee camp to have “work at home” and lockdown? Say you did have a surveillance system in that setting, and you identify an outbreak of COVID-19. There is no ICU [intensive care unit]. There are no ICU doctors. There are no ventilators. What exactly is the appropriate action item arising from that surveillance system? Even with the best data, even with the best analytics, if your intent is to have a public health impact but there are no public health interventions available, then what are you trying to achieve with your science?
This has been a personal struggle for me. Writing a paper that results in a scientific article is all well and good. You can do the best science possible with the data you have and produce the best risk map, for example. But if you want to make a difference in the real world, among the populations that you care about—in my case, vulnerable populations—if there is no intervention resulting from even the most rigorous surveillance, then what are we doing?
I’m deeply worried about global health and the poorest populations. They are going to be crippled by this pandemic, because of famine, crushing poverty, mental health problems, humanitarian aid pipelines drying up.
We will see measles and polio outbreaks because vaccination programs have been paused. Infectious disease is not like other kinds of disease. If you lose traction for a year, then you’ve lost control of the whole thing. Controlling malaria, for example, requires constant and continuous application of interventions. One year of letting up, and you’ve lost years and years of progress. That’s the nature of infectious diseases, because they’re nonlinear. COVID, of course, is a terrible crisis. But losing ground against other pathogens is going to come back to bite us.
•••
At the beginning of the pandemic, everything I did was very operational. I felt it was my duty. I was working basically day and night, day and night—no break—for months. During this time, a lot of women felt that they wanted to do helpful things. So we weren’t applying for grants. We weren’t writing papers. Meanwhile, men in our institutions were getting lauded. They were on every panel and podcast, while we were just trying to get work done.
One night, I wrote a letter to Times Higher Education. It was published in May, under the headline “Women in science are battling both COVID-19 and the patriarchy.” I wrote it after a glass of wine, because I was so angry. I wrote it in a fit of rage, and it was meant to be just me. But I thought it would be better if we had lots of women weigh in. I reached out through Twitter, where groups of women researchers had started to form. I said, “Hey, does anyone want to sign on?” There was this massive amount of interest. In the end, 35 women scientists signed.
Interestingly, quite a few women said, “I love that you’ve written this, but I just can’t be an author.” They felt they would be troublemakers, and it wouldn’t look good. I already am a troublemaker. And I don’t care. The fact is that I’ve proved myself scientifically. I have a big, productive group. I’ve brought in money.
We need to have at the table people who know how to get things done. Very often, those people are women. I think that individual women’s careers will regress after this pandemic, because a lot of us have been doing operational work instead of writing papers, so we will appear to come out of this crisis without scientific products to show for it. At the same time, a lot of us have been home with children and still playing the major role in child care.
I have a quantitative research group, and it’s mostly women. That’s quite unusual. Within my group, the women have felt marginalized and spoken over and have witnessed more sexism from outside our group than they’d been aware of before. That makes me sad, because I think a lot of them will choose to leave science.
I feel a responsibility to my students and my postdocs—to show them that you don’t have to be apologetic and grateful all the time. Even in a crisis like this pandemic, I feel a responsibility to raise these issues, to speak out and be brave about these things. Because, well, who else is going to do it?
first responder

Paul Biddinger
Director, Emergency Preparedness Research Evaluation and Practice Program
Medical Director for Emergency Preparedness,
Mass General Brigham
The mindset of a first responder is to intervene and help. They want to be the first there. They want to be the first to make the situation better. They want to be on the sharp end of the spear.
What makes a great first responder? That’s a good question. Calm. Especially as a leader, keeping a level head is extremely important. If you get really worked up, you start yelling and start moving, everyone feeds off it, and the whole thing goes out of control. By the same token, if you’re calm, if you project an air of capability, then it changes the tenor of things.
As soon as we started seeing serious outbreaks spreading across China outside of Wuhan and outside of China—they happened almost at the same time—it was pretty clear the coronavirus infection was going to be a worldwide problem. We’d been preparing our hospital for years to be able to handle a case of anything. But for managing the actual patient surge, we had not turned on our emergency plans like that since the Boston Marathon bombings in 2013. The marathon was a big one for us. But there has been nothing like the pandemic, in terms of scope, scale, actions required—nothing.
•••
I don’t want to sound melodramatic, but the burden of keeping everybody safe—about 26,000 people at MGH [Massachusetts General Hospital], 78,000 across Mass General Brigham—in the context of not knowing much about the disease was enormous. We were looking every single day at every published article we could find. Personal protective equipment, our donning-and-doffing training, our protocols for how you enter and exit a room, meeting after meeting after meeting, trying to reassure people, trying to explain what we know and be honest about what we didn’t know: All that was huge. It was a level of stress unlike anything I’ve ever felt.
It’s hard to see friends and colleagues so anxious. How did I reassure them? First and foremost, it has to come from the relationship and the trust that we built over the years—that they trust that I really do care an awful lot about them and would never, ever knowingly put anybody in harm’s way. No one wants to have any suspicion in their mind that a decision is being made for a financial or for an expeditious reason. They need to know and trust that we’re doing what we do because of what we know about the science and because we put our staff first. Ultimately, for a lot of people, what was reassuring was showing them our own data. Here’s what we are seeing in terms of health care workers becoming ill, transmission of the disease, why we think our approach is safe.
We had huge teams of people come to the Emergency Department to help out. On days when we were intubating five or 10 or more patients a day—critically ill patients—a team of physicians, nurses, and respiratory therapists would all descend every time a patient entered a room. Volunteer or redeployed staff from elsewhere in the hospital would stay outside—they were support runners. If somebody needed a piece of equipment, they’d run and grab it, they’d grab a medicine. It was like a pit crew at a Formula One race.
•••
You asked what did it feel like. I’m sorry, because some of these answers tend toward the dramatic. I tried to leave the command center and walk the halls and get out in the hospital whenever I could, to keep in touch with what people were thinking and feeling and experiencing.
During those times, I saw a sense of purpose that was extraordinary. An intensive care unit is normally a pretty active, noisy place. In the early months of the pandemic, it was actually quieter than usual—even though, on average, patients were even sicker than they normally are. Just the look in people’s eyes, the way they were doing what they did—it’s a feeling that’s hard to describe. There was this competent, calm, purposeful feeling.
•••
I think that most all of our staff feel extremely proud of their response. By that, I mean that they feel that they were supported and they were able to deliver the extraordinary care they’re capable of delivering. They were able to do what they needed to do to save lives. Ultimately, I think, they felt protected.
One of our intensive care physicians made a really important comment. It was a point when we had hit about 80 deaths overall in our ICUs. Our mortality rate compared very favorably with what was being reported elsewhere—and we knew we had really delivered a lot of care. You might think it was possible to look at the 80 number and say, “Isn’t it great that we’ve only had 80 deaths?”
Her comment was, “But it’s 80 deaths. Each one takes an incredible toll on the staff, on the unit—and of course, on the family of the person who died.” We’re not free of tragedy, of sadness—people who had to die alone in the hospital because we didn’t permit visitors. You can’t forget that. The two things come together.
There are some apartment buildings next to the hospital on the way to where I park. The first time that I left the hospital at 7 p.m., people were clapping and cheering. That was—sorry. [Tries to compose himself. Takes a few deep breaths.] It was amazing. Definitely something I’ll remember for my whole life. [Tears well in his eyes.]
That one hit me pretty hard. It was a recognition of the struggle and the gratitude. The cheering was clearly meant for all the people at the bedside, all the people who showed up, all the people who did what they needed to do, even if they were scared themselves.
Bridge Builder

Chi-Man (Winnie) Yip
Professor of the Practice of Global Health Policy and Economics
Director, Harvard China Health Partnership
My family lives in Hong Kong, my mother and siblings, so I keep up with Hong Kong and Chinese news. Toward the very end of December, I was in Boston, reading a Hong Kong newspaper. It said that there were cases of pneumonia with an unknown cause. It also said that experts hoped it was not another SARS.
In my mind, I was thinking, “Oh, I hope it isn’t. But if it is, China will have much more experience in dealing with it, given China’s experience with SARS and the public health infrastructure built afterward.” So I sort of pooh-poohed it. But by the time I landed in Hong Kong in early January—I was visiting our collaborators in China to plan this year’s work and visiting my family in Hong Kong for Chinese New Year—it was on the front page of the newspaper.
The SARS memory is a strong imprint in people’s minds in Hong Kong. Maybe because Hong Kong people have gone through SARS, when you have a newspaper on the front page alluding to something similar to SARS, people turn on their radar, their brain. They’re preparing.
My mother, who’s 85 years old, said, “Why don’t we just buy some masks?” We went first to Watson’s. It’s a chain that is similar to CVS here. They had sold out. They said, “Come back in the morning. We usually have about 20 boxes, but they sell out in an hour.” Then my mother and I walked by a pharmacy. The owner said, “I can only sell you two boxes.”
My meetings with the National Health Commission and the WHO’s China office were canceled. They told me that they were very busy dealing with the situation in Wuhan. I was surprised that what was happening in Wuhan was not on the radar of the common people—including our collaborators in China.
Chinese New Year was early this year—on January 25. The Wuhan lockdown was the 23rd. I was beginning to feel that fear and scare momentum building up. People tuned in to the news on an hourly basis for updates: Wuhan is locked down. Which cities would be next? Is Hong Kong closing its border? Meanwhile, we tried to have a normal Chinese New Year. When I left, on the second day after Chinese New Year, the airport in Hong Kong was almost empty. In that huge departure hall, which usually holds thousands of people, there were 10, 20 people.
•••
There’s a community spirit that I thought China had lost because of so many years of market forces and capitalism. During the coronavirus, that spirit reemerged. That’s the heartwarming part.
Locking down a city is a top-level policy decision. But in Wuhan, the epicenter of the epidemic, the healthier, younger people voluntarily went to do grocery shopping. They would identify older people, high-risk people, and they delivered food to them. They would drive people who needed to seek care. These self-initiated actions, responding to the needs of your neighbors, I just find it very moving. This is not top-level government saying that you have to do X, Y, Z.
What is the source of that generosity? I think that deep down, Chinese are very—maybe Confucian is the right term, because in Confucianism you care about your community, your neighbors. That sense of community still exists in people’s hearts. Most of the time, society is driving people toward achievement and earning more money. This unexpected crisis brought out that deeper part of individuals. How do we bring that out when the crisis is past? This is my intellectual question right now. That sense of community is critically important in my work to revitalize primary care in China.
•••
I see myself as a bridge between China and the U.S., not with the political leaders but with colleagues—academics or think-tank researchers in health systems, health policy. I try to help each side clarify their misunderstanding of the other side.
One thing that I kept hearing in the U.S. was that China purposefully was hiding the facts. There is some truth in that. But I don’t think it is the whole story. In the time between when a doctor started noticing suspicious cases to the final decision to lock down, it was Western New Year, which was observed in China, and then Chinese New Year. People were getting ready to have this great holiday. There was a sense of wrapping things up.
Chinese New Year is a big thing. I sometimes challenge my U.S. colleagues and say, “Imagine that everybody is preparing for Thanksgiving. Then imagine something 10 times more significant than Thanksgiving. Everybody’s preparing to go home. Migrant workers, who work so hard for a year—this is the time they go home for reunions.”
At that time, we didn’t even know whether the virus’s transmission was animal to human or human to human. We didn’t know the incubation period. We didn’t know how infectious it was. For the Chinese government to announce, “We’re having a crisis, everything stop”—just think about that. I would call that government irresponsible if the problem turned out to be something not so serious. This lack of clarity prompted me to organize a seminar in March called “Decisions During Uncertainty.”
•••
Now, many people in China also misunderstand the United States. They draw conclusions based on what they read or hear in the media. From their perspective, if China could control the spread of COVID-19, why couldn’t the U.S. follow the same strategies? They interpret it to be a malfunction of the American government. In one sense, they are right. But they also don’t understand many other fundamental causes in the U.S. health care system, the decentralized decision-making system, American social structure and culture. I think understanding each other more would help both sides have a healthy conversation. It’s not about who is right or wrong but working together to find a better future.
Most of my Chinese colleagues see the U.S. as a failure, if I may use that word, in managing and controlling this pandemic. For them, that failure has been revealing. It revealed to them that there are fundamental weaknesses in the country.
But Chinese people also felt a little bit of disappointment, because despite the tense U.S.-China relations at the political level, many still look up to the United States as the leading country that they can learn from. So there’s disappointment—a disillusion. In China, wearing masks is not about obedience, as Western media sometimes portray Asian culture—it is about how “my” action affects society at large. For my Chinese colleagues, and even for my family in Hong Kong, to hear that the U.S. needs to debate whether or not to wear masks, it’s almost beyond their comprehension.
engineer

Michael Mina
Assistant Professor of Epidemiology
Faculty, Center for Communicable Disease Dynamics
Associate Medical Director in Clinical Microbiology,
Department of Pathology, Brigham and Women’s Hospital
In January, the writing was on the wall. There was no way this virus was not going to hit the U.S. From an infectious-disease-dynamics perspective, it had already demonstrated an amazing capacity to spread within China and quickly to Thailand and other places. I said to my bosses at the Brigham that we need a test. They had reservations.
Over the next couple of weeks, the Biogen conference outbreak occurred and people started realizing that we did need a test. [The conference, held in Boston in February, led to some 20,000 COVID-19 cases in the Greater Boston area by early May.] The FDA [U.S. Food and Drug Administration] was dragging its feet. It became exceedingly apparent, early in February, that there was no way, even if we got a test running, that we would be able to test enough people. Maybe we’d get a hundred or 200 tests going a day. That wasn’t going to be enough for Massachusetts or even for our hospital system.
That led to my working with the Broad Institute. It’s a very academic place, but it almost runs like a corporate entity. It’s not driven by money but by this insatiable need to be efficient. I had contacted an infectious-disease researcher and clinician there named Deb Hung. We started talking. She put me in touch with her colleagues who normally run the genetics platform.
The Broad’s good at a lot of things, but one thing it’s exceptional at is scaling tests. The moment we started talking, they said, “What would it take to get a PCR test?” None of them had done PCR for viruses. They did human genome sequencing, which is a very different thing, but at the same time uses a lot of the same robots and same tools. Almost overnight, before I even knew what was happening, they were jumping on it. I talked to them for the first time on a Monday. By the next Monday, they had already started building walls and setting up a new BSL-2 [biosafety level 2] laboratory.
It felt like forever, but it was two, two and a half weeks from the time that we started planning to the time when we had a workable roboticized assay on which we could start running samples. It was light speed.
If you remember at the time, the CDC had to recall all their test kits. The state lab had almost no capacity—they were running maybe 10 or 50 tests a day and already completely overflowing. At the Broad, we built capacity for 30,000 tests a day. It is one of the single highest-capacity laboratories in the country at this point.
•••
To me, this epidemic is bringing out what needs to happen in the future. Everything that has gone wrong with testing should not be brushed under the rug, should not be forgotten. Our biomedical industry and public health industry are burdened by red tape and lack of money and complexities in reimbursements and who’s doing what and when. What it shows me is how inefficient our current practice of medicine is.
To make real change, we have to build relationships with industry and with engineers. In college, I trained as an engineer. Today, I see that everything that’s gone wrong with the testing situation in this country and in the world has been engineering problems or people problems—but people problems can be engineered. We need engineers, and people who think like engineers, at the helm, because it’s a throughput problem. That’s what the Broad experience showed. They knew nothing about the biology of this virus, but very quickly, almost overnight, their mechanical engineers and people who think like engineers were able to make a high-throughput laboratory.
When I went to the Brigham and said I want to get this thing started with the Broad, my boss said, “Michael, you have great ideas, and when you have them, you’re usually right. But you’re too inexperienced to know that what you’re proposing is impossible.” That, to me, says it all.
•••
Technology has made it so cheap to do antibody testing that, with just a small amount of blood or saliva, we have an opportunity to create something like an immunological observatory. You can also get antibodies out of donated plasma and blood. The surveillance can be very efficient. The goal is to build an immune observatory lab in each country or each continent. You could ramp these up. One lab doing millions and millions of tests a year wouldn’t be a huge ask.
If we had been doing this kind of surveillance in New York City back in January or February, even if we didn’t know that the coronavirus was an emerging infection, we would have detected aberrant signals—cross-reactive antibodies. These are antibodies from previous infections that might be elicited by this new pathogen and that would have binded to this pathogen. We would have pretty quickly seen, “Hey, this is interesting, we’re starting to see a big increase in antibodies against coronaviruses in a pattern that we haven’t detected before.” That would have told us there’s a new pathogen out there.
If you want to do a rapid test for antigens in an active infection, you just enroll people and have them spit every day into a tube of saline solution and insert a small piece of paper embedded with a strip of protein. If they are infected with enough of the virus, the strip will change color within 15 minutes.
The government needs to stop looking at individual companies and asking, “Who’s making the best rapid test right now?” They need to ask instead, “What is a technology that works that can be done cheaply?”—and then just start making it themselves in the same way that they print money or do anything else. For everyone to be testing themselves every day with results in five minutes—especially in the hot spots right now—that would go a long way to stopping this epidemic in the U.S.
I try to follow what I think are important things that either need to be done or that could change society. I don’t think I’m visionary. I think I’m practical.
Physician/
scientist

Sarah Fortune
Chair, Department of Immunology and Infectious Diseases
John LaPorte Given Professor of Immunology and Infectious Diseases
I’m from Lexington, Kentucky. My grandfather was a local community physician at a time when being a community physician meant wholehearted dedication to one’s community. I only knew him as an older person, so I didn’t see all the sacrifices that entailed. What I did see was how deeply enmeshed in his community he was. I could not go anywhere as a kid—my last name’s Fortune, it’s recognizable—without someone saying, “Oh, you must be related to Dr. Fortune. He took care of somebody in my family.”
I graduated from college in 1990, and I started medical school at Columbia in 1991. At that time, there was another great pandemic: HIV, prior to the advent of antiretrovirals. If you went into Columbia Presbyterian Hospital, two floors were the HIV and TB [tuberculosis] wards—because at that time, there was a TB epidemic in Manhattan that actually was on par with TB statistics in some parts of sub-Saharan Africa. That was the crisis of the moment, the compelling scientific and moral biomedical challenge.
Recently, I’ve been thinking a lot about family histories. On my father’s side, a distant cousin was the first female graduate of the University of Kentucky. My great-grandfather was a minister in the Disciples of Christ, and he was tried for heresy in 1920, because he was not a strict textualist and he believed in evolution. My father was a law professor, and every seven years, he took a sabbatical and worked as a public defender. So I come from a family where there’s a tradition of service and commitment to intellectual ideals. Bringing intellectual curiosity to bear for societal good.
•••
I’m an infectious-disease doctor. I’m a TB researcher. But even for somebody like me who understands the dynamics of infectious diseases, it’s hard to shake an intrinsic sense of American exceptionalism. It seemed like surely the federal response to the pandemic would be swift and overwhelming, and that we would stamp out the coronavirus domestically. Instead, we’re reacting to the dynamics of the virus, as opposed to anticipating the dynamics of the virus and then planning such that it doesn’t get out of hand.
Life is uncertain, right? We go through life as if we understand what’s going to happen tomorrow, and it’s only when really big things happen, catastrophic things, that you realize you have no certainty about what’s going to happen tomorrow or the next week or the next week after that. In our own lives, there’s willful denial of this all the time.
The thing that makes the profession of science different is we are very front and center about uncertainty. We say, “Here are the knowns. Here are the unknowns. And here are the known unknowns.” But even the things that we pitch as known, there are ripples in the data that suggest that maybe everything is not exactly as known as we think it is. In fact, when people go back and say, “Does the biology really work that way?” you’d be astonished at how many times what is known is just a sort of construct placed over our best guess—a construct that is, in and of itself, inaccurate.
For me, the thing that has been most surprising about this virus has been how it presents. There is a whole range of clinical manifestations that we used to refer to as fuzzy “post-viral syndromes”: chronic fatigue syndromes, neurologic syndromes, Kawasaki syndrome. We would say, “Oh, that’s just post-virus.” If you’re really honest, for some of those patients who had post-virus symptoms, we thought the problem was psychosomatic.
Now, with COVID-19, it is very clear all of those cases were post-viral. You see the epidemiology. You’re like, “Wow, this is amazing,” because you understand the full clinical manifestation of both a viral illness and the recovery from a viral illness. The coronavirus’s post-viral symptoms are temporally rolling through populations. The clinical road map to how complicated the immune response to infection is, and how long it takes your body to reacquire equilibrium, is suddenly very interesting.
Aside from that, the biology of the coronavirus has been within the bounds of predictable or understandable. It’s the political and societal manifestations that have been astonishing. It’s been astonishing and sad that we have not had a more coherent national dialogue and response. There were many paths that we could have taken. Sweden has taken one path. New Zealand has taken another path. Germany, another. I don’t pass judgment on any one of those paths, except to say that they had a strategy at a public health level, and we have not.
•••
You did not ask about the other major societal happening this year—the deaths of George Floyd, of Breonna Taylor, and the recognition of where we are as a country in terms of race and racism.
I became department chair in January. So for me, this moment—in the context of a pandemic that is clearly affecting communities of color much more severely than other communities—has changed how I think about science. We’re a department that studies TB, HIV, malaria, and emerging pathogens like SARS-CoV-2. These are diseases of Black and brown people around the world, right? Yet we have no Black faculty. About 4 percent of the graduate students at Harvard are Black. We have to do better.
Understanding the convergence of these two moments has changed how I think about my responsibilities to my lab, my local community, and to the broader scientific community. It’s a front-and-center priority. If you look at who’s doing the research on COVID, it’s white and Asian scientists. It’s not scientists from the communities that are hardest hit. For an academic community that likes to think itself very liberal and progressive, we have real problems and we need to fix them.
Drum beater
Yonatan Grad
Melvin J. and Geraldine L. Glimcher Assistant Professor of Immunology and Infectious Diseases
Faculty, Center for Communicable Disease Dynamics
There’s a wonderful book by Philip Fisher called Wonder, the Rainbow, and the Aesthetics of Rare Experiences. He writes about wonder as an exclamation—as in, “What a wonder!”—and wonder as an interrogative, as in, “I wonder how that works?” I have always found that to be one of the more succinct summaries of why I love science. There’s a beauty to it.
But beauty is just half of it. The other half is a sense of moral imperative to do good in this world. That’s a large part of why I went into medicine. I also see public health as a way to unite the delight in science with that moral imperative. I became interested in infectious diseases because the questions that they raise are about how people interact with each other and the world around them. Anthropological, sociological, philosophical questions: They all play out in infectious diseases. And those questions get amplified in a pandemic.
•••
Once we had a model of how SARS-CoV-2 might spread, I was very interested in a basic question: What would happen if we had lockdowns of varying duration and success in reducing spread? That was a question where you run through the numbers, you look at the figures, and it hits you what we’re up against.
The driving concept is that the pandemic only ends under a couple of scenarios. One is that we eliminate the virus through containment—that is what happened with SARS in 2003. But from early on, when we were starting to see spread of SARS-CoV-2 globally, it became clear that the infection was not going to be something that we could control and eliminate. So the second option was herd immunity. And the way we could get to herd immunity was either through a vaccine or through enough of the population getting infected and developing sufficient immune protection so that reinfection would be prevented.
In early March, we were looking at what we might see with the pandemic going forward—four-week, eight-week, 12-week distancing interventions of varying success. Our models showed that we’re in this for the long haul, this thing isn’t going away, and also that, to the extent that a one-time social distancing intervention was successful in preventing spread, we would expect to see the virus return when we stopped social distancing, because as long as there are enough susceptible individuals to sustain virus spread, in the absence of other types of mitigation efforts, it will spread. That’s why you end up needing multiple rounds of distancing. This is a drum we’ve been trying to pound for months—this was clear back in March.
•••
We all understood that the political and social will to do multiple rounds of distancing was unlikely. But there was dismissiveness even among people who study infectious diseases. It was hard to convince them that this is not like seasonal flu, that there is no immunity in the population to this virus, that this thing is going to spread. We didn’t know what the true infection fatality rate was, but Wuhan was such a clear example of the devastation the virus can cause. Northern Italy was another example. I was floored by how many infectious-disease experts saw those examples and just did not get that the virus can do the same thing wherever it goes—including in the U.S. This was an easy extrapolation from things that were widely reported.
I want to point to our political system right now. How are people ignoring the obvious? There’s wishful thinking or some inability to project into the future and anticipate what will happen. This is, I think, one of the themes of the pandemic. Epidemiologists and modelers would say, “Cases are going up. That means hospitalizations and deaths will follow. You cannot make policy decisions based on what you see today. You have to project, based on exponential growth, weeks or months into the future. You have to anticipate what will be.” But people find reasons why that is not the case.
A lot of us have felt burned out recently. Because you beat the drum—it’s almost Cassandra-like. It’s not even just that you’re trying to predict the future. You just point to the past and say, “This is what happened in Wuhan. This is what happened in Lombardy. This is what happened in New York. Why would you think you’re any different?”
•••
People like to contrast modeling with weather forecasting. The pandemic is not a hurricane, where you batten down the hatches and wait for it to pass. The pandemic is shaped by what we do. We have a choice. We can actually shape our experience. So to see the criminal abdication of responsibility by the federal government has just been—boy, it has been and continues to be the hardest thing around so much of this. I have lost a lot of sleep over it. That’s another contributor to burnout.
In the spring, it felt right to put pretty much everything on hold and focus. One of the things that has been amazing about this experience is the sense of camaraderie, standing shoulder to shoulder with friends and colleagues I admire and working together. But this is also a call to arms, right? It’s a call to service. You mentioned the sharp elbows in academia. This felt far more important than any individual accolade. One of the reasons I wanted to be at a school of public health is because the moral compass is clear. Yes, it’s about the beauty of the science. But it’s also about trying to do good.
globalist

Barry Bloom
Joan L. and Julius H. Jacobson Research Professor of Public Health
Former Dean, Harvard T.H. Chan School of Public Health
The first papers about the pandemic came out near the end of January—one in the Lancet, the other in the New England Journal of Medicine. Both were published by Chinese scientists I knew who, remarkably, had trained at Harvard. The Lancet paper summarized clinical data from Wuhan, essentially describing the disease to the world so that any physician could see it. The New England Journal paper put out the first epidemiologic model indicating that this was going to be a terrible pandemic. Seeing two papers from Chinese scientists so soon after the virus emerged, I just thought that was extraordinary.
I had been invited to China in 2003, when I was dean, after SARS had broken out. It was clear that China had failed in addressing the problem of SARS, and they were looking for ways to do better next time. I and my colleagues noted three failures in the system. The first was that the science was absolutely weak. The second was that communication amidst the public health systems across this giant country was completely chaotic. The third was the inability to communicate the risks in a reasonable, safe, honest, and transparent way, yet in a way that did not panic the public.
China did tremendously better at the science level this time than in 2003. What one has to appreciate is that things have really tightened up in China in terms of scholars’ freedom and ability to speak one’s mind. This spring, I published two pieces in Forbes to try to protect the good scientists there, who were being trashed by both the U.S. government and the Chinese government.
Early on, these scientists were under tremendous pressures about what to make public. We read in newspaper articles that they were criticized: Why did you publish in the two top journals in all of biomedical science? Why didn’t you publish in a Chinese journal? They were extremely visible and vulnerable. We need to protect the people who were doing the critical science from attacks from within and from without, and make it clear the international scientific community depends on their production of knowledge and information.
•••
We know—published in the New York Times, spoken on television—that the head of the CDC received a call from the head of the Chinese CDC on January 3rd announcing that China had atypical pneumonia that was infectious. The Chinese alerted us to it, perhaps not at the earliest possible time but certainly in time to begin to prepare for its arrival here, because we know flus that originate in China always come here.
There was a time when we had 47 representatives of the CDC with an office in China. They were almost all pulled back. I went on the website recently. It says there are three assignees at the China office now, but it doesn’t say that they’re there. Had they been there last December, it would have been inconceivable they would not have known what was going on in Wuhan. They were good. I met them often when I went to China, and I went to China every year for many years. We regrettably had no eyes on the ground.
So there was a failure at every level to respond to an approaching epidemic. We knew what was coming. Epidemiologists at the Harvard Chan School and Johns Hopkins knew what was coming. Many, many scientists knew what was coming, and nobody could get through. There is no scientific capacity in the White House.
You can’t deal with scientific problems in a government that doesn’t believe that there’s climate change or where there is no central government health care system. That’s not a way to protect the country from a tragic epidemic.
There was a Gallup Poll in 1996 that asked a representative subset of the American people: Would you pay a dollar a week for biomedical research? Seventy-seven percent said yes. Although probably they didn’t know what biomedical research meant, they knew that good things came from it. A subsequent Gallup Poll asked: Do you know what public health is? Seven percent said yes, and Gallup didn’t query further whether the respondents did actually understand the term.
Nobody paid any attention to public health until 9/11 and anthrax. After that, public health was something that you started to read about in the newspapers. Then with water pollution, atmospheric pollution, climate change, it got into a broader realm. But the punch line is, if we do everything right in public health, there’s nothing to show, which is why it’s hard to get funding. It’s a fact that, in all of the epidemics that I’m aware of, the money was thrown at public health only after it was too late. We don’t invest until after a disaster occurs.
•••
How do I cope with the failures of this pandemic? Just sadness. Sadness that there is so much knowledge that could be brought to bear that would save lives and the economy. Sadness that no one cared because the knowledge came from elite colleges and elite people called scientists. That’s not new. To be honest, when I was a college student, I took a summer course for fun at Harvard taught by H. Stuart Hughes. The title of that course was “Anti-Intellectualism in America.” That’s an American tradition. Too many in the U.S. want people in government at the middle- to lowest-possible level of integrity and expertise. You don’t want them to be better than you. That’s not true in all countries.
I like to say that all health care is local, all health research is global. But today, the name of the game is that whoever gets there first gets all the marbles—we live in a country that is fighting to keep everything American and nationalistic and populistic. But the international nature of science—the need for openness, transparency, and collaboration—is more essential now than ever. With this pandemic, scientists have been sharing their unpublished information to the extent that an archive was created because journals can’t move quickly enough. That’s revolutionary. That’s never happened before. From the scientists’ point of view, that’s been transformative.
One of the ancient Confucian values is reciprocity. If you take the lofty view that all science is global and all research is global, then we need collaboration. We need each other.
leader

Michelle A. Williams
Dean, Harvard T.H. Chan School of Public Health
Angelopoulos Professor in Public Health and International Development, Harvard Chan School and Harvard Kennedy School
There’s an old Jamaican saying: You can teach the kid that the stove is hot, and most kids will listen, but some have to feel the heat before they understand.
We in public health have long been making a strong case for investment in pandemic preparedness and response. But only now with the pandemic, when we’re close to the heat and seeing these preventable deaths mount, do we realize that we have deep systemic flaws in our public health systems, our supply chain, our health communications, our data structure, our data systems. And the recent sequence of convulsions—the pandemic, the economic fallout from the pandemic, the George Floyd killing—all shine a light on the ugly underbelly of structural racism and inequity in this country.
This is a public health moment. But ever since the pandemic started to unfold, I’ve reflected that moments can’t just be moments. Public health has to be a sustained movement.
I just completed my fourth year as a dean. I’m at my core a person who doesn’t seek the limelight, who wants to do the job, recognizing that as dean of a school I have to be out front. This pandemic has made me redouble my efforts in being out front. It has made me more, I would say, emphatic about what is public health, why is public health. It has made me want to describe in every opportunity I have the places where public health has been undersupported, not given its due respect. If I miss this moment to explain the primacy of public health in the economic and national security of our nation and all nations, I will feel as though I have missed an opportunity for our discipline and for society writ large.
So yes, the pandemic has changed me. It’s added a sense of urgency to my work. It’s made me shed my desire to stay in my comfort zone, just out of the glaring light. And it has stoked the determination to be heard and to be even more supportive of other public health leaders and students who are going to be leaders one day. I want to tell them: We can’t be timid in public health.
•••
When George Floyd was killed, my siblings and I started to talk. We’re all distant geographically right now. I’ve got a sister in Maryland, a sister in Pennsylvania, a brother in North Carolina. The only converging we did was by text messaging and by telephone. We reflected on growing up in a home where we had, in the middle of our living space, a classic picture—we’re children of the ’60s and ’70s—of Martin Luther King, Bobby Kennedy, and John Kennedy. We were talking about this photo. We grew up in a household where we would think about the civil rights leaders and those who enabled our Jamaican parents and us to enjoy some of the liberties that got us to where we are, even as we realized that we have a long way to go.
For me, the murder of George Floyd was the low point. I was already physically and emotionally tired from my public health work on the COVID-19 response, fighting and supporting and working long days. Both of my sisters are nurses, and one of them was laid low by COVID. She was infected at work and ended up spending 14 days in hospitals, 10 of them on a ventilator. And then during a 24-, 36-hour period, seeing the story of Christian Cooper in Central Park, in the city where I grew up, and witnessing those eight minutes and 46 seconds of George Floyd’s last moments: I felt like the bottom dropped out—the earth just fell out from under my feet.
I’m 58 and I’ve worked 30-plus years. I’ve encouraged other Black and brown people the same way my parents encouraged us. The world’s unfair, but don’t wait for it to become fair. Expect to work twice as hard. Expect half as much. But it will change one day because of what you and others around you do. Seeing George Floyd murdered the way he was, I felt that my whole life’s work didn’t count for much. It certainly didn’t in the last eight minutes and 46 seconds of his life. That changed me. That was my bottom.
Reading helps me escape the reality and go to a place where I can find room to reflect. I read Toni Morrison’s The Origin of Others, this beautiful little work. Toni asks fundamental questions: Why is it that we as humans are so afraid of others? Why do we even create othering? Why do we promote the creation of othering through race? We’re one human race. She asks these questions, and we should be asking ourselves these questions and working actively against racism now and until we accomplish the goal.
•••
Very close friends, when I considered taking the role of dean, said, “Michelle, the world needs you now to be the dean. You are the dean for the moment.” I didn’t understand that at the time. I am understanding it more so now. For me to be the dean of the moment, I have had to change the way I conduct myself as a leader. If I’m going to make someone uncomfortable by saying “racism” and by talking about the disproportionate impact of COVID-19 on Black and brown people, it should be done compassionately and effectively. I will not miss the opportunity to call out injustice when it exists.
It’s not that I’ve ever been or ever will be a craven dean, but there are everyday pressures not to rock the boat, not to self-advocate for public health too much. That’s no longer the kind of dean that I will be. I will be direct. I will be compassionate. And I will be a stronger advocate for public health.
messenger

Bill Hanage
Associate Professor of Epidemiology
Faculty, Center for Communicable Disease Dynamics
I’ve been having nightmares since January. In January, the nightmares were this sense that there was this way through the data, but I wasn’t able to find a path. I’d be tossing and turning, and I’d have a moment of hope at some point that I really understood things. Then I wouldn’t be able to figure out why I really understood them. By the end of February, March, I was having this sense of huge quantities of death.
More recently, quite a lot of the nightmares have been to do with physical distancing. I’ll be at something and I’ll be talking to somebody. Then I’ll realize that I shook hands with them and I shouldn’t have. Or I’ll see a whole bunch of people and I’ll be trying to keep away from them. There was one occasion—I think it was in March—when I woke up my wife, Helen. I was talking in my sleep about physical distancing. She could tell from the tone of my voice I was dreaming that I was talking to a reporter.
•••
I feel that my personality has changed since February. At first, I just sat there looking at outputs of things and torturedly eyeing them and wondering what was going on and doing rough calculations and having Twitter conversations and direct messages. The change that happened in February was that I realized that I had to take action. Many of us had this notion that, somewhere, clever people were doing the things that we thought were obvious and should be being done. We were naive.
So I started taking a more proactive approach. I started thinking, “OK, what do I know about the virus? I know this about the virus. I’m going to have to get out ahead of it.” I changed my Twitter bio to have the pinned tweet as saying, “Don’t panic. Do prepare.” I thought that was an important message.
Before this pandemic, in my entire life, I had written one op-ed. Most of the time, I think and write in cool, deliberate ways. But the op-ed in the Guardian, which was the first one about the pandemic that I published there, was written in about an hour. The headline was: “I’m an epidemiologist. When I heard about Britain’s ‘herd immunity’ coronavirus plan, I thought it was satire.” The government was doing virtually nothing to stop transmission of the virus and wheeling out scientists to state that this would build up the population’s herd immunity. My op-ed was published on March 15. On March 17, the prime minister, Boris Johnson, announced that he was reversing the herd immunity policy—although whether or not it was actually the policy is unclear, even today.
In the U.K., leaders were also talking about the idea that, at a certain point, older people would need to protect themselves. We were saying, “But how?” Around that time in early March, we were talking to my in-laws, who live in South London. We urged them to stay indoors. “Sorry, we know that sounds silly. We know it sounds ridiculous. Don’t go outside. Get things delivered. Just please don’t leave your home.” It may have saved their lives.
We’ve lost family friends to the virus. We know what it can do. I know many of the victims are old, but I think about the tens of thousands of bereaved men and women quarantined while getting used to being on their own, after years being together with their beloved. Having to say goodbye on FaceTime, followed by a socially distanced funeral, which only two people could attend. I am savagely angry about that.
•••
There’s a sports bar literally around the corner from our home. It’s called Parlor Sports. There’s a particular table, which a friend calls the corner office. I will sit there and watch soccer. It was in Parlor Sports that I finished up my contribution to a paper about the effectiveness of various interventions in Wuhan. It was one of my last visits.
My last visit to Parlor Sports was on a Sunday early in March. I went in there quite late. I stood at the end of the bar and sort of gestured to the bartender, who’s a friend of mine—like me, he’s an Arsenal fan. He came over and said, “What’s up?” I said to him, “I’m here to tell you”—he knew what I did for a living—“that things are going to get really bad, and they’re going to get really bad really soon. I want you to know, because you’re my friend and because I want you to be prepared.” He poured me a shot. We both did a shot. He said, “See you.” I said, “Yeah, see you. I’ll look forward to it, whenever it is.” I went home, and when I came in, I washed my hands for 20 seconds and changed my clothes.
Now Parlor Sports has reopened as a takeout restaurant doing soft-serve ice cream and burgers from a window on the street. I can go there to see my friend and chat, distanced. I support the business as much as I can. You don’t want things to go bust. You don’t want your community destroyed by this pandemic.
•••
I’ve long had something of an obsession with the work of Albert Camus. In fact, if you look up my Twitter account, there’s a lot of Camus-related commentary. It took me three months, but I reread The Plague.
There is a huge amount of wisdom in that book, and among it is that you have to keep going, exhausted as you are, and that the most important thing in fighting the plague is—it’s translated as “decency” in the most common translation, but the actual French is l’honnêteté, which is not simply honesty. It suggests to me a bunch of other things, including straightforwardness and down-to-earth-ness and humility in the face of it.
Various people have said, “This is the moment you’ve been preparing for your entire life.” I’m not sure I quite agree with that kind of grandiloquence.
A few years ago, I lost my best friend to cancer. It was a horrible time. It was, up until now, easily the most difficult time in my life. But it didn’t have any professional component. It was entirely personal. And being able to communicate some of the medical facts to his family felt like I was helping.
At his funeral, I was asked to give the eulogy. They got me into a church—it was amazing. I gave the eulogy, and as we were walking away, one of his colleagues came up and complimented me on it and said, “That must have been very hard.” My immediate response was, “Thank you very much, but it was not nearly as hard as not doing it.” I feel the situation now is like that.
Madeline Drexler is editor of Harvard Public Health







