[ Spring 2013 ]
Microbes in and on our bodies outnumber human cells 10 to 1—and may determine how we get sick and stay well.
The story of public health has largely been a story of conquering infections, from smallpox to syphilis to scarlet fever. Since the late 19th century, the War on Germs has boosted life expectancy and eased incalculable suffering.
But today, scientists are realizing that the unseen bacteria, viruses and other microorganisms that pervade our world are not necessarily our foes. While our bodies contain some 10 trillion human cells, there are more than 100 trillion microbial cells in and on every exposed surface of our bodies—a resident menagerie collectively known as the human microbiome. (Because of their small size, microorganisms make up only 1 to 3 percent of the body’s mass.) And while we sport about 23,000 human genes, our microbiome contains some 8 million, making them a far more capable force than we had ever reckoned.
Put simply, our bugs are us. And according to Curtis Huttenhower, assistant professor of computational biology and bioinformatics in the Department of Biostatistics, that insight may transform our understanding of how healthy bodies become diseased, how aging leads to infirmity and especially how we might tinker with our internal ecosystems to prevent and treat a vast range of conditions, from diabetes to asthma to obesity.
“Our relationship with our microbes is not a war; it’s a well-defined truce, a balance. It’s a system that natural selection has worked on for millions and millions of years,” he says. “We get one genome and that’s what we’re stuck with for our life. But our bugs can change and adapt much faster than we can. And our immune system, our metabolism and many other systems in our bodies evolved specifically to engage in this rapid conversation with our bugs, and vice versa.”
Now, for the first time, scientists are listening in.
Power in numbers
In the long genealogy of life on Earth, single-celled microbes preceded multicellular creatures by a billion years. According to Huttenhower, “You could say that humans and other multicellular organisms evolved as robots to carry around microbes.”
And microbes can boast power in numbers. “If you go to Africa and count the large mammalian species, it’s in the double digits, but their interactions and ecology are still complex,” he explains. “If you examine a particular skin location or a microbial biofilm in the mouth, you’ve got ten or a hundred times that many different kinds of bacteria, all interacting, and each with its own niche and genome and priorities.” The human gastrointestinal tract is the most microbially diverse part of our bodies, exposed to an onslaught of foods, drugs and other disturbances that exert strong and constant selection pressures.
In 2007, the National Institutes of Health launched a massive five-year consortium to map our microbial complexity. The agency’s Human Microbiome Project (HMP) created a base line portrait of a healthy human microbiome. By sequencing more than 5,000 samples from 242 healthy volunteers in two U.S. cities, it revealed the contours of microbial diversity in disease-free individuals. Researchers sampled and analyzed the genomes of microbes from five areas on the human body: nasal passages, oral cavities, skin, the gastrointestinal tract, and the urogenital tract.
The project found that more than 1,000 microbial species occupy our internal ecosystems. And while our human genomes are more than 99 percent identical genetically, our microbial communities are typically only about 50 percent the same. That suggests that different species of bugs are doing the same jobs in our bodies—in a sense, pinch-hitting for one another.
On and in each person
|
The HMP also found that while the worst bad guys—microbial pathogens—aren’t present in healthy individuals, all of us carry organisms that can cause disease under the wrong circumstances. Most of the time, these “opportunistic” pathogens live in harmony with their human hosts, providing the vital functions necessary for their and our survival. How and why these microbes become renegades rather than team players is an important scientific question.
New tools and technologies
These insights were made possible by new tools, both in the lab and on the computer. Traditionally, microbiology has focused on single species, often isolating each by itself in a petri dish for examination. But the vast majority of microbes that thrive in and on us have never been cultured in this way, in part because their growth depends on a particular microenvironment that had not been, or could not be, replicated at the bench.
Modern advances in DNA sequencing technology changed all that. Today, scientists can parse not just the genome of a single bacterial strain, but the genetic material from whole microbial communities. They first purify the human and microbial DNA in a sample straight from the environment, sequence it and then use computers to sort through the resulting genomic fragments and identify the genetic signals found only in bacteria and other microbes. This cheap, high-volume technology can create an instant catalog of organisms, genes and genomes from a microbial community sample. “From literally billions and billions of microbial DNA sequences,” says Huttenhower, “we’re beginning to interpret these complex mixtures of nucleic acids—the A’s, C’s, G’s, and T’s—in terms of how they affect our ecosystems and our health.”
 A lead author for one of the HMP papers published in Nature, Huttenhower likens the possibilities to those that suddenly opened when astronomers began using radio telescopes. “The data that you obtain from a radio telescope aren’t something you can see with the eye, but abstract values read out of an instrument and converted into a pattern by a computer. Likewise, in biology, we’ve gone from optical microscopes—our equivalent of telescopes—to instruments that rely on DNA sequencing and use a computer to tease out signals from the data.” Using these high-throughput sequencing technologies, researchers have uncovered an infinitesimal universe.
A lead author for one of the HMP papers published in Nature, Huttenhower likens the possibilities to those that suddenly opened when astronomers began using radio telescopes. “The data that you obtain from a radio telescope aren’t something you can see with the eye, but abstract values read out of an instrument and converted into a pattern by a computer. Likewise, in biology, we’ve gone from optical microscopes—our equivalent of telescopes—to instruments that rely on DNA sequencing and use a computer to tease out signals from the data.” Using these high-throughput sequencing technologies, researchers have uncovered an infinitesimal universe.
Unique microbial profiles
Each of us has a unique microbial profile—in some ways, our bugs are as much a biological signature as our genomes. Our unique sets of microbial passengers are forged by genetics, early life events, diet, and a lifetime of exposures to infections, pharmaceuticals and other aspects of our physical environment.
Even within each of us, individual body sites harbor unique microbial ecologies. “To the microbes living on our bodies,” says Huttenhower, “our skin and our mouth and our gut are as different as a desert and a prairie and a rainforest.”
Conditions that may someday be treated by altering the microbiome
|
Where do these organisms come from? Until birth, humans are virtually sterile, consisting of only our own somatic cells. But during the first few years of life, we are bathed in microbes we pick up from our mothers, the hospitals where we’re born, our homes, our families, food, clothing, trees, dirt, pets, playgrounds, the air we breathe. Some of these organisms stick with us all our lives, while others are transient.
Just as these microbes need us to survive, we rely on them as well. Among other things, they train our immune systems from an early age to discern healthy flora from disease-causing invaders, break down our food into nutrients that we can absorb, manufacture essential compounds such as vitamins and anti-inflammatory signals, and crowd out dangerous pathogens, such as disease-causing strains of Clostridium difficile in our intestines or Staphylococcus on our skin.
From health to disease
And when this ecosystem, finely tuned by evolution, slips out of balance, we get sick.
Inflammatory bowel disease (IBD), for example—a group of conditions that includes Crohn’s disease and ulcerative colitis, both painful and relapsing conditions—seems to be triggered when normal gut bacteria become less diverse and shift in their proportions of various species. Huttenhower is working on a study that may illuminate whether the typical high-fat, low-fiber Western diet correlates with the microbiome profile found in IBD patients. To help answer that question, he is drawing on data from the Health Professionals Follow-Up Study, which for a quarter-century has collected detailed information on volunteers’ diets and lifestyles. Using oral and fecal samples from the study’s volunteers, Huttenhower hopes to learn how IBD, a disease with both genetic and environmental components, interacts with microbial influences in the environment.
What microbes do for us
|
Other autoimmune conditions, such as type 1 diabetes, rheumatoid arthritis and asthma, may also arise from changes in the microbiome. Long before researchers began investigating the microbiome, they knew that allergies and asthma were tied to early-life environments. Children who are more exposed to dirt and animals are less likely to develop allergies and asthma. The so-called hygiene hypothesis suggests that childhood exposure to germs and certain infections trains the immune system to be robust later in life, and that, conversely, relatively clean environments in early life prod the immune system to overreact to harmless substances such as pollen.
Microbiome studies may uncover the mechanisms behind the hygiene hypothesis. Today, researchers are comparing the microbiomes of children raised on farms and exposed to livestock with those of kids who grow up in cities. According to Huttenhower, “If you’re a child in an urban area that’s all steel and concrete, with no trees and no parks, that increases your risk of allergy or asthma later on, relative to growing up in open areas with more natural microbial communities.”
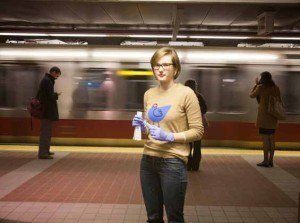
Microbes and mass transit
In 2012, Huttenhower received a grant from the Alfred P. Sloan Foundation to study how our normal microbial communities are transmitted during our everyday lives, such as in Boston’s crowded MBTA subway system. Swabbing samples from subway cars and touch screens on three different lines, his team will try to find out how or if bugs are transferred between people, becoming permanent denizens of other riders’ microbiomes.

communities are transferred in daily life. Below: A student swabs a touch screen in Boston’s crowded MBTA subway system.
“What happens when I shake somebody’s hand?” he ponders. “Do their skin microbes get beaten out, in some sense, by my skin microbes, because my microbes have evolved to be with me? Or do our microbial communities combine? Or do they stably transfer some of their community to me? And do those same patterns of transmission hold true for surfaces and airways? That’s why I’m interested in looking at the MBTA: How do our bugs get to our environment and back, if at all?”
Given the intimate connection between our microbiome and our own cells, other conditions, from obesity to mental illness to the frailty of old age, are also ripe for exploration. Huttenhower cites several recent studies indicating that the microbiome in older people, for example, is less diverse than in the young. As in several other conditions, this raises the question of whether changing microbial communities are a cause or a result of declining health during aging and disease.
Into the clinic?
Microbiome studies may someday pay off in methods to alter the course of disease. According to Huttenhower, “An important difference between our microbial genes and our own genes is that our microbes are plastic and modifiable. Every time we eat something or take antibiotics, we change our microbial communities. This means that they have the potential to be an effective point of prevention and disease treatment.”
Take the painful and seemingly random flare-ups of Crohn’s disease. “If we could determine from changes in bugs—say, from a stool sample or, in an optimistic world, a saliva sample—that there’s a microbial or immunological change before the flare begins, then we could treat the problem before it starts,” says Huttenhower. That treatment could consist of standard medications, or perhaps even of tailored doses of bacteria that would restore the gut microbiome to a healthy state. (Think of it as a research-based version of consuming large quantities of live-culture yogurt to keep the digestive system functioning smoothly.)
Deploying bacteria as drugs isn’t new. Earlier this year, studies showed that transplanting fecal specimens from healthy individuals cured Clostridium difficile infections—an agonizing and sometimes deadly infection in the intestine, usually in the elderly, that typically follows a regimen of broad-spectrum antibiotics. Indeed, antibiotics—the lifesaving medications behind many of public health’s 20th-century triumphs—may turn out to have unintended consequences beyond the well-documented problem of drug-resistant pathogens.
If our bodies are composed of delicately balanced microbial environments, then antibiotics are like a “wildfire,” says Huttenhower. “They burn down everything.” Even interventions like fecal transplants “are a big hammer,” he conceded. “A question many of us are interested in is: What’s the smallest, most targeted, most nuanced intervention to treat not only C. diff infections or IBD, but also other inflammatory conditions such as diabetes or rheumatoid arthritis? Could we introduce a single species of bacteria, or just a few species, to restore a healthy, diverse ecology? Could we target specific molecules or a specific chain of events in microbial communities, the way we’ve begun to do in cancer?”
The microbiome even offers possibilities for early diagnosis. “We should be able to learn to read our bugs to tell us about our future health, just like we’ve done with the human genome in the past 10 or 15 years,” says Huttenhower. Microbial profiles are potential clues to whether patients will respond to drug treatment, need surgery or stand the risk of ever developing certain diseases.
But it’s important to temper the enthusiasm of the moment against the daunting challenge such research presents. “Think about how long it’s taken us to find molecular treatments for cancer or genetic treatments based on the human genome, both of which have been more studied by more people for a lot more time,” he warns. “All translational science underestimates two things. One is the difficulty of reliably picking a signal out of big data. The second is the difficulty of going from that signal to the clinic.” Both steps are possible in the human microbiome, but neither will be easy.
High stakes
But the stakes for such research are high, and the potential payoff dramatic. “The microbiome is one part of the environment that might help explain the rapid increase in the last 50 or so years of chronic, nongenetic disease. Obesity, types 1 and 2 diabetes, inflammatory diseases like inflammatory bowel disease, and autoimmune diseases like rheumatoid arthritis have all have gone up at a rate that cannot be explained by human genetics, and therefore must be caused by changes in our environment,” Huttenhower says. “Changes in that time have included diet, our stress levels, our indoor and outdoor environments, and our use of antibiotics and other pharmaceuticals. All of those factors also affect our microbiomes, which have evolved over hundreds of millions of years to train our immune systems and keep us healthy. The last few decades have seen changes at a rate faster than anything else during those millennia, and our microbes might be having trouble adapting—putting our health at risk in the meantime.”
If those connections prove true, he adds, “That’s a huge motivation to do this work. We need to focus on this now, as quickly as possible.”
Madeline Drexler is editor of Harvard Public Health.
Download a PDF of Our bugs, ourselves here
