As the AIDS epidemic tragically demonstrated, public health has usually been a step behind infections on the run. But today, with sophisticated molecular and communications tools, practitioners can virtually keep up stride for stride with emerging epidemics.
In the spring of 2003, a deadly viral illness—severe acute respiratory syndrome, or SARS—swept out of China’s Guangdong Province and spread rapidly around the world. HSPH professors of epidemiology Marc Lipsitch and Megan Murray, using a sophisticated mathematical model to estimate the virus’s potential to spread, showed that the most effective means of blocking SARS transmission would be to isolate infected individuals and quarantine people likely to be exposed—strategies that, along with preventing transmission in hospital facilities, successfully contained the startling new epidemic.
In the early spring of 2009, H1N1 influenza—the same subtype, though milder, that killed an estimated 50–100 million people worldwide in 1918—emerged in Mexico and swiftly spread around the globe. Lipsitch statistically modeled the severity and transmission of the virus, while Atul Gawande, professor in the Department of Health Policy and Management, led a World Health Organization team to quickly draft a patient care checklist for hospitals managing suspected or confirmed cases.
In May and June of 2011, a novel strain of E. coli, dubbed O104:H4, triggered a brief but deadly outbreak of foodborne illness centered in Germany and France. In one of the first uses of whole-genome sequencing to study the dynamics of a foodborne outbreak, a team led by HSPH researchers and the Broad Institute traced the deadly path of the outbreak, which killed more than 50 and sickened thousands.
And in the past few years, Caroline Buckee, assistant professor of epidemiology, has developed predictive models for the spread of malaria, using anonymous cell-phone data to track the movement of people in malaria-endemic regions. “Cell phones are ubiquitous,” she said. “Using them to monitor people’s mobility during an outbreak could transform infectious disease epidemiology.”
The human microbiome
Mapping the future
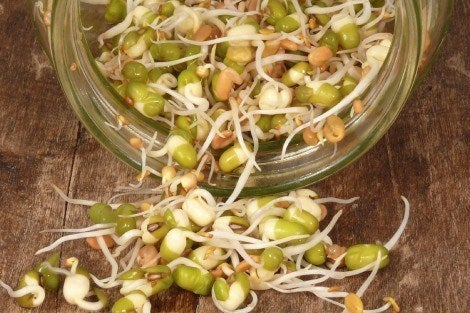
 Helping to write the next chapter of infectious disease research, Curtis Huttenhower, associate professor of computational biology and bioinformatics, is exploring the human microbiome—the 100 trillion microbial cells in and on our bodies. Research on the microbiome may transform our understanding of why we become sick and how doctors may someday tinker with our internal ecosystems to prevent or treat a vast range of conditions, from diabetes to asthma to obesity. “Our relationship with our microbes is not a war,” said Huttenhower. “It’s a well-defined truce.”
Helping to write the next chapter of infectious disease research, Curtis Huttenhower, associate professor of computational biology and bioinformatics, is exploring the human microbiome—the 100 trillion microbial cells in and on our bodies. Research on the microbiome may transform our understanding of why we become sick and how doctors may someday tinker with our internal ecosystems to prevent or treat a vast range of conditions, from diabetes to asthma to obesity. “Our relationship with our microbes is not a war,” said Huttenhower. “It’s a well-defined truce.”