May 9, 2013 — A new study has shed light on why a monkey malaria parasite that typically caused only mild infection in humans is now beginning to cause severe disease and death—and how it has the potential to become a dangerous human-to-human pathogen. In a multidisciplinary study using experimental and modeling approaches, researchers at Harvard School of Public Health (HSPH) showed that while the parasite usually prefers only young red blood cells, it can adapt over time to invade both younger and older cells—thus greatly increasing its virulence.
The study appeared March 27, 2013 online in Nature Communications. Senior authors were [[Manoj Duraisingh]], associate professor of immunology and infectious diseases, and [[Caroline Buckee]], assistant professor of epidemiology at HSPH.
“We are excited to be able to culture this parasite for the first time in human red blood cells, but also to explore the population-level implications with mathematical models,” said Duraisingh. “This study identifies a likely mechanism for virulence evolution of a recent human parasite.”
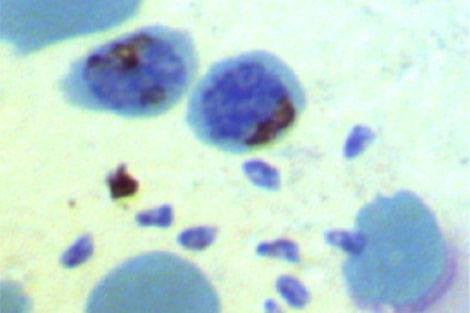
The study is the first to provide a mechanistic explanation of the virulence of Plasmodium knowlesi, a macaque malaria parasite. This parasite usually proliferates poorly in human blood because it prefers only the youngest of red blood cells. (Red blood cells live for three months in the bloodstream.) But after studying the parasite in the lab and using mathematical modeling—an interdisciplinary approach that brought together experts in epidemiology and immunology and infectious diseases—researchers showed that, over a four-month period, the parasite can develop the ability to replicate efficiently in older red blood cells as well.
The parasite’s ability to adapt over time to thrive in older red blood cells as well as young ones—an adaptation with a likely genetic origin, the researchers say—may make P. knowlesi increasingly dangerous for humans. High levels of the P. knowlesi parasite in the blood could cause individuals to develop severe and possibly lethal malaria. High blood parasite levels also increase the risk that P. knowlesi could become a human-to-human pathogen. Given these findings, P. knowlesi in humans should be closely monitored in the future, the researchers said.
While cross-species transmission of malaria parasites is rare, human activities in Southeast Asia such as logging and farming have led the macaque malaria parasite to become a “zoonosis”—an infection that jumps from animal to human. “The public health importance of zoonoses is increasing as habitat destruction and climate change continue to expose human populations to pathogens of wild animals,” Duraisingh said.
By providing the first mechanistic explanation of the virulence of P. knowlesi, this study generates a good working hypothesis for why some individuals suffer from severe disease with this strain. “Our model suggests that this type of adaptation could be an important determinant of virulence for other malaria parasites as well, including Plasmodium falciparum, the type that causes the most deaths,” said Buckee.
The team was also able to create new ways to culture the P. knowlesi parasite in the lab, which will enable further study of the parasite’s biology. “This work provides an important model system for studying malaria,” Duraisingh said. “The parasite can be grown in human red blood cells and be widely accessible to the malaria community.”