April 15, 2016 — On April 13, the Centers for Disease Control and Prevention (CDC) joined the World Health Organization (WHO) in confirming a link between Zika and the severe birth defect microcephaly. While officials at WHO also believe that there is enough evidence to conclude that the virus causes the autoimmune nervous disorder Guillain-Barré syndrome, the CDC is waiting for the results of additional studies.
Last year, the Zika virus—a mosquito-borne pathogen first identified in 1947 and never before seen in the Western Hemisphere—erupted in Brazil and has since spread to more than 20 countries in the Americas. The outbreak raised new questions about how the timing of infection in utero affects fetal neurological development, whether vaccines should be tested in pregnant women, and how the scientific energy generated during public health crises can help basic research uncover hidden mechanisms of human biology.

Eric Rubin, the Irene Heinz Given Professor of Immunology and Infectious Diseases at Harvard T.H. Chan School of Public Health, spoke recently about the outbreak with Madeline Drexler, editor of Harvard Public Health and author of the book Emerging Epidemics: The Menace of New Infections.
Zika, chikungunya, dengue, West Nile virus, Japanese encephalitis: All of these infections jumped to the Western Hemisphere in recent years from far-flung parts of the world and are now permanently established. What does that tell you?
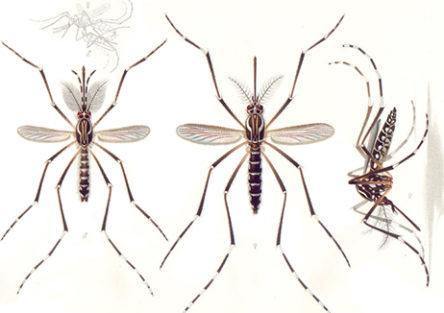
That mosquitoes are a great way to spread disease. When you transplant a disease into a new area with the right mosquito vector, it can spread like wildfire. In the case of both chikungunya and Zika, it’s probably that people have no natural immunity and that both of those infections are being transmitted by the same mosquito—Aedes aegypti, which is extremely well-entrenched in these areas.
What are your biggest scientific questions about Zika?
First, what is the risk to the fetus in pregnant women? Are the brain abnormalities such as microcephaly and other conditions in the fetus happening in 1 percent of infections or 100 percent of infections? If women get infected early in pregnancy, is that better or worse than late in pregnancy? Finally, is asymptomatic infection associated with risk to the fetus? If it is, then this outbreak will be even more of a disaster than it already is.
Second, are there other health issues in the children of mothers who were infected—problems that are less severe than microcephaly, more subtle abnormalities such as developmental delays? And do we know for sure that other syndromes are associated with Zika infection, such as the Guillain-Barré syndrome?
What are the challenges in designing a vaccine for Zika?
In theory, one should be able to make vaccines against flaviviruses, such as dengue or Zika. They’re simple viruses, their immunity is understood. The biggest challenge is making a vaccine that’s safe. In particular, is it safe in the target population for the vaccine: pregnant women? If you target young women or women just before or at childbearing age, then you have to be sure it’s safe in pregnancy. We don’t tend to test new drugs in pregnancy. The National Institutes of Health has been pushing the idea that pregnant women should be included in clinical trials, but it is understandably frightening to do that.
Does Zika infection produce long-lasting immunity? That would be important if we were to make a vaccine for it. And if Guillain-Barré syndrome does occur with the infection, introducing the antigen in the vaccine could induce the same neurologically damaging autoimmunity.
For decades, we’ve been hearing that the next devastating pandemic will spring from a bird flu in Asia. But actually, the latest human-transmitted flu, in 2009, came out of North America. No one predicted SARS. No one predicted Zika. Why are emerging infections so hard to forecast?
They’re inherently unpredictable because of human behavior. For flu—which is going to be the great pandemic and when it arrives will kill more people than any other infection—there’s a lot of random chance involved. There are already risky human behaviors taking place, such as living in close proximity to birds, growing fowl for food. There is also a set of genetic mutations and recombinations that will produce a virus that’s highly virulent and efficiently spread from human to human. It’s completely predictable that all those pieces will fall into place. But you have no idea when, because there are so many random events that have to happen. That’s the part that is chance.
You are both a physician and a microbiologist. What can you learn from an outbreak like this?
Why do you become a scientist? It’s because nature surprises you all the time. It’s not unpredictable that Zika virus could spread and could infect a lot of people—but that it would have these consequences was surprising. Why does Zika virus infect the brain of the fetus? If it doesn’t infect the adult brain, why not? Answering those questions might give us an idea of the differences between the developing brain of the fetus and the fully formed brain of infants and children, who don’t seem to be affected in the same way.
From pathogens like Zika virus, we also learn a lot about fundamental human biology, because they’re probes of our own physiology. Microbes exploit our vulnerabilities. They take advantage of the normal processes that occur in us and subvert them. In many cases, we didn’t know that those normal processes even existed until they got subverted. Emerging infections like Zika virus help us better understand ourselves.
Photos: E. A. Goeldi, Len Rubenstein