Study finds presence or absence of chronic conditions key to health-related quality of life
For immediate release: Thursday, April 21, 2016
Boston, MA – Do survivors of childhood cancer return to normal health as they grow up? According to new research from Harvard T.H. Chan School of Public Health and Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, overall health-related quality of life in young adult survivors of childhood cancer resembles that of middle-aged adults. In a study published today in the Journal of the National Cancer Institute, the investigators show that childhood cancer survivors who are 18 to 29 years old report overall health–related quality of life similar to that reported by adults in the general population who are in their 40s.
The key variable determining people’s sense of well-being is the presence or absence of chronic health conditions. Childhood cancer survivors have been found to have higher risks of heart disease, infertility, lung disease, cancers and other chronic conditions related largely to their prior chemotherapy, radiation, and surgery. Examining health indicators in 18-to-49 year-olds who participate in the national Childhood Cancer Survivor Study (CCSS), the investigators found that only 20 percent reported no chronic conditions. As survival of childhood cancer has increased substantially since the 1970s, research has expanded into ways to reduce the toxicity of treatment to minimize late effects as well as cure the disease. Although a number of pediatric cancers are now treated with less intensive therapies, aggressive treatments with high toxicities remain part of care.
“This research provides an easily accessible way to compare adult survivors of childhood cancer to the general population, in terms of their health-related quality of life, which normally declines as people age,” said Lisa Diller, MD, chief medical officer of Dana-Farber/Boston Children’s and the study’s senior author. “Our findings indicate survivors’ accelerated aging and also help us understand the health-related risks associated with having had cancer as a child. What’s encouraging is that the lower quality of life scores are associated with chronic disease after treatment, not with a history of pediatric cancer itself. If we can prevent treatment-related conditions by changes in the therapy we use for the cancer, then childhood cancer will become an acute, rather than a chronic, illness.”
The JNCI study is the first to use the Medical Expenditures Panel Survey (MEPS) to compare the health-related quality of life of the general population with that of childhood cancer survivors. The survey’s household component, which includes questions on health status and demographics, has previously been used to compare the self-reported overall health of people in the general population and those with specific conditions, such as liver disease, chronic pain or HIV/AIDS. In addition to utilizing MEPS, the researchers included information from CCSS on siblings of childhood cancer survivors. The sibling findings matched the MEPS results.
Using health status data collected from adult CCSS respondents age 18-49, researchers assigned health-related quality of life scores in which 1 indicated perfect health and 0 indicated death. They found that childhood cancer survivors who reported no chronic health conditions had scores similar to the general population. Survivors with chronic conditions had scores that matched the scores of chronically ill members of the general population.
Findings include:
- Early decrements in health-related quality-of-life were observed: Young adult survivors, age 18-29, had an average health-related quality of life score of 0.78, on the 0-1 scale, roughly equivalent to that reported for 40-to-49 year-old adults in the general population.
- The more chronic conditions, the lower the score: Childhood cancer survivors with no chronic conditions had an average health-related quality of life score of 0.81. Those with two chronic conditions scored lower, at 0.77.Those with three or more disabling, severe, or life-threatening conditions had an average score of 0.70.
“By enabling comparisons to the general population, our findings provide context to better understand how the cancer experience may influence the long-term well-being of survivors,” said Jennifer Yeh, PhD, lead author of the study and a research scientist in the Center for Health Decision Science at Harvard Chan School. “This is another way to understand the health challenges survivors face and where to focus efforts to improve the long-term health and quality of life of survivors.”
The MEPS sample consisted of 12,803 individuals. The CCSS sample included 7,105 survivors of pediatric cancer and 372 siblings.
The research was supported by the National Cancer Institute and the American Lebanese-Syrian Associated Charities.
For more information:
Todd Datz
Harvard T.H. Chan School of Public Health
617-432-8413
tdatz@hsph.harvard.edu
Irene Sege
Dana-Farber/Boston Children’s Cancer and Blood Disorders Center
617-919-3110
irene.sege@childrens.harvard.edu
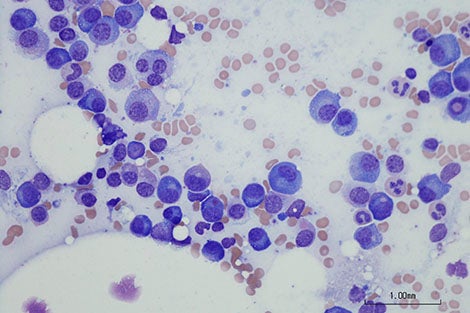
photo: iStockphoto.com
###
Harvard T.H. Chan School of Public Health brings together dedicated experts from many disciplines to educate new generations of global health leaders and produce powerful ideas that improve the lives and health of people everywhere. As a community of leading scientists, educators, and students, we work together to take innovative ideas from the laboratory to people’s lives—not only making scientific breakthroughs, but also working to change individual behaviors, public policies, and health care practices. Each year, more than 400 faculty members at Harvard Chan School teach 1,000-plus full-time students from around the world and train thousands more through online and executive education courses. Founded in 1913 as the Harvard-MIT School of Health Officers, the School is recognized as America’s oldest professional training program in public health.
Dana-Farber/Boston Children’s Cancer and Blood Disorders Center— the nation’s top pediatric cancer center, according to U.S. News & World Report 2015-16. – brings together two internationally known research and teaching institutions that have provided comprehensive care for pediatric oncology and hematology patients since 1947. The Harvard Medical School affiliates share a clinical staff that delivers inpatient care at Boston Children’s Hospitaland most outpatient care at Dana-Farber Cancer Institute.