Introduction
The escalating epidemic of obesity and type 2 diabetes is intersecting with infectious disease epidemics in many low- and middle-income countries (LMICs), leading to widespread multi morbidity for patients and massive challenges for health systems. Countries in sub-Saharan Africa (SSA) are particularly vulnerable to the emerging epidemic of diabetes given their nascent health systems. The Lancet Diabetes & Endocrinology Commission will provide a comprehensive analysis of the growing diabetes burden and the challenges faced by countries of SSA, health system responses and the gaps that need to be addressed in care and prevention of obesity and diabetes in SSA. The Commission will involve key policy makers, funders, clinical leaders and academic institutions as well as civil society organizations, healthcare industry, and institutions concerned with diabetes.
What are the objectives of the Commission?
- To ensure that diabetes care and prevention – which intersects with maternal and child health and infectious diseases —is appropriately prioritized in SSA health systems.
- To provide frameworks and the evidence necessary at all levels to enable health systems to provide high quality, cost-effective care to all diabetes sufferers in SSA.
- To provide recommendations for health systems interventions that will start to halt and reverse the tide of obesity and type 2 diabetes in SSA.
Why is the Commission needed?
- Both type 1 and type 2 diabetes are areas of urgent clinical need in SSA. Patients with type 1 diabetes require frequent access to essential medicines and structured health care. Lack of such access means that for many sufferers in SSA – particularly children – type 1 diabetes is a death sentence. Most patients with type 2 diabetes also have poor access to good quality care, resulting in a high rate of life-threatening complications, for which patients also lack access to care. More than 60% of patients with diabetes in SSA are undiagnosed, meaning that there are more patients unaware of their disease in SSA than in any other region in the world. Improved infrastructure will enable better surveillance, diagnosis, education, and access to care and medicines.
- As type 1 diabetes is often fatal in young people in SSA, and young people are increasingly affected by type 2 diabetes, poor access to care and essential diabetes medicines has substantial effects on countries’ economies. Young people affected by diabetes and its complications are often unable to work and provide for their families. Thus, investing in effective diabetes treatment and prevention will provide a net benefit to a country’s economy.
- The prevalence of obesity in SSA is already at moderate to high levels. In SSA, diabetes currently affects 10.4 million people, 3.1% of the total population. The number of persons with diabetes is predicted to rise to 18.7 million (3.5% of the population) by 2025. The projected rapid economic growth, urbanization and social transitions which are bringing about changes in lifestyles and nutritional habits have the potential to markedly increase rates of obesity and type 2 diabetes, as observed in countries of Latin America and the Middle East that have recently undergone such changes. The globalization of lifestyle and food habits that accompany investment by food industries may exacerbate this problem.
- Despite the increasing prevalence of diabetes and obesity (in addition to other non-communicable diseases (NCDs)), these areas are relatively neglected in the public health arena in SSA, and are in need of urgent funding. Increasing awareness of and funding for NCDs in SSA is essential to ensure that they have a firm place on the public health agenda.
- Most of the SSA countries with weak health systems and fragmented services for different diseases are not equipped to deal with the burgeoning levels of chronic diseases in general, and diabetes in particular. As good diabetes care cuts across many healthcare disciplines, improving care for those with diabetes offers the opportunity to strengthen weak health systems
How will the Commission address its work?
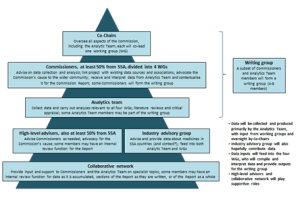
The Lancet Diabetes & Endocrinology Commission is co-chaired by Prof Rifat Atun (Harvard T.H. Chan School of Public Health) and Prof Edwin Gale (Bristol University) and includes approximately 15 additional Commissioners. Commissioners are focused into four working groups, which are supported by an analytical team, as shown in the figure below.
The Commission will convene three in-person meetings of the Commissioners, at the start and midway points for in-depth discussions of the Commission’s work, and at the end of the process, to discuss the findings of the Commission and how to translate them into action in the real-world setting.
The analyses undertaken by the Commission focuses on six main areas:
1.) Current and projected burden of diabetes: An in-depth exploration of individual, household, health system and societal burden of diabetes will be undertaken, accounting for presentations of diabetes (both type 1 and type 2) which appear unique to SSA. The differing requirements of children with type 1 diabetes and of adults developing type 2 diabetes in urban and rural settings will be highlighted.
2.) Risk factors leading to obesity and diabetes: Early developmental factors exacerbating type 2 diabetes (in particular, early life under-nutrition and later life over-nutrition), interactions with other diseases prevalent in SSA, and the sources and sustainability of food production will be explored. The Commission will also address diabetes and obesity as risk factors for other NCDs.
3.) Resources and health systems: Current practices and preparedness of health systems in several countries will be analyzed to ascertain their readiness in managing diabetes and NCDs, to identify innovations in prevention, clinical care and control of diabetes, and determine the challenges experienced in providing public health measures to mitigate against obesity and appropriate to treat diabetes and its complications. Exploring means to improve access to cost-effective, evidence-based management will be a central objective. We will identify where health systems can learn from successful models of care – for example, integrated care models or community-based approaches that have been introduced for management of infectious diseases.
4.) Gaps in knowledge and care: Gaps in knowledge needed for effective management of diabetes in SSA, and the gap between what is needed to manage the existing and future burden of disease and the resources available to do so, will be identified.
5.) Cost-benefit analysis: A thorough cost-benefit analysis will be done to highlight to policy makers where the most beneficial investments should be placed for maximum gains at individual, household, health system and societal levels.
6.)Identifying future actions: The Commission will identify actions with targets and milestones for introducing preventative measures to reduce levels of obesity, and for strengthening health systems to effectively manage diabetes and related chronic illnesses. We will also recommend measures to ensure future accountability in managing the diabetes epidemic in SSA.
Output
The Commission will produce a 30,000 word report, peer-reviewed by and published in The Lancet Diabetes & Endocrinology. This report will provide a reference point for all stakeholders involved in improving health systems in SSA, establish a framework for action aimed at enabling health systems to provide services that are efficient, cost-effective, and commensurate with the burden of disease from obesity and diabetes and set milestones for future actions.