March 14, 2018—Scientists at Harvard T.H. Chan School of Public Health demonstrated a new vesicle-based system for delivering molecular cargo into cells—a discovery that may significantly improve targeted drug delivery.
The study was published online March 6, 2018 in Nature Communications.
Extracellular vesicles (EVs) are the cell’s shipping containers. These microscopic, membrane-bound capsules are secreted out of cells and loaded with molecular cargo—think DNA, RNA, hormones, or proteins— which gets shuttled to neighboring cells or to cells in other tissues.
Scientists had tried to engineer EVs that deliver drugs directly to diseased cells, but with limited success. Then in 2012, a research team led by Quan Lu —associate professor of environmental genetics and pathophysiology and senior author on the new study—revived hope for vesicle-based drug delivery with their discovery of ARMMs, a new type of EV with novel properties.
In 2017, Lu’s team showed that ARMMs could ferry NOTCH receptors—signaling molecules involved in cell-to-cell communication—to faraway cells. It was a novel discovery, as NOTCH wasn’t known to signal at a distance. But ARMMs upended the conventional wisdom. They could transport NOTCH between non-adjacent cells, where ARMMs would home in on their target, then jettison their cargo into the cell on arrival. Even before publishing this finding, Lu recognized that ARMMs could be repurposed for drug delivery.
“We hypothesized that if you could swap out the signaling molecule and swap in a therapeutic molecule, you could potentially use ARMMs to deliver macromolecules—DNA, RNA, proteins—for therapy,” Lu said.
To test this, Lu and his research associates Qiyu Wang and Jiujiu Yu—lead authors on the new study—engineered ARMMs to deliver p53, a tumor suppressor protein that responds to and repairs DNA damage. In cases of extreme damage, p53 triggers apoptosis—a genetic kill switch that destroys irreparably damaged cells. Mutations in p53 can hinder its ability to respond to damage, a defect in the cell’s innate defenses that may turn the cell cancerous. But Lu thought he could use ARMMs to introduce normal p53 into damaged cells and resuscitate their impaired defenses.
Lu was right. ARMMs carrying p53 (p53-ARMMs) offloaded their cargo into human cells and activated damage-response genes. But Lu’s team went a step further. They engineered ARMMs to deliver p53 mRNA—the molecule cells use as a template to produce the protein—which activated the same damage-response genes as the protein itself.
Still more impressive was their effect on genetically engineered mice incapable of producing p53. The mice were injected with p53-ARMMs, then exposed to high doses of radiation—doses that induce apoptosis in normal mice. The p53-deficient mice wouldn’t be expected to activate apoptosis after irradiation. But those injected with p53-ARMMs did. The results show that p53-ARMMs can compensate for missing or damaged p53.
The researchers also engineered ARMMs to deliver fully functional CRISPR-Cas9—the much-hyped genome editing technology—into human cells carrying an active copy of the green fluorescent protein (GFP) gene. GFP glows green under UV light. But CRISPR inactivated the gene and suppressed the green glow in these cells. Since CRISPR can be tailored to target any DNA sequence, scientists hope to use it to cure genetic diseases like Tay-Sachs or sickle-cell anemia—a feat that requires getting CRISPR into diseased cells. Though delivery systems already exist, Lu thinks ARMMs might provide a major advantage over the existing options.
“We think we can engineer the surface of ARMMs with homing signals,” Lu said. “Potentially, you could package CRISPR, or any other molecule, and deliver it to any tissue of your choice.”
Though the study was intended as a proof-of-principle demonstration, Lu said it’s just a first step. His lab is actively developing homing signals that would direct ARMMs and their therapeutic cargo to diseased cells. It portends a future where ARMMS could deliver CRISPR directly to lungs to treat cystic fibrosis, chemotherapy to kill only cancer cells, and other innovative therapies that clinicians now only dream of.
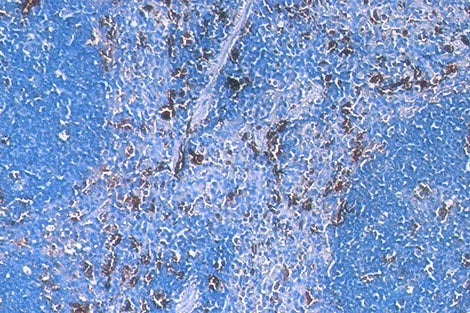
Image courtesy of Quan Lu