At a time when America is largely relying on the internet for their jobs and education, about one-third of rural households report serious internet connectivity problems.
For immediate release: October 7, 2020
Boston, MA – During a time of record-setting growth in new COVID-19 cases across rural America, a new NPR/Robert Wood Johnson Foundation/Harvard T.H. Chan School of Public Health poll finds that about one in four rural households (24%) report household members have been unable to get medical care for serious problems when they needed it during the coronavirus outbreak. A majority of these households with anyone who has been unable to get care when needed (56%) report negative health consequences as a result (see Figure 1).
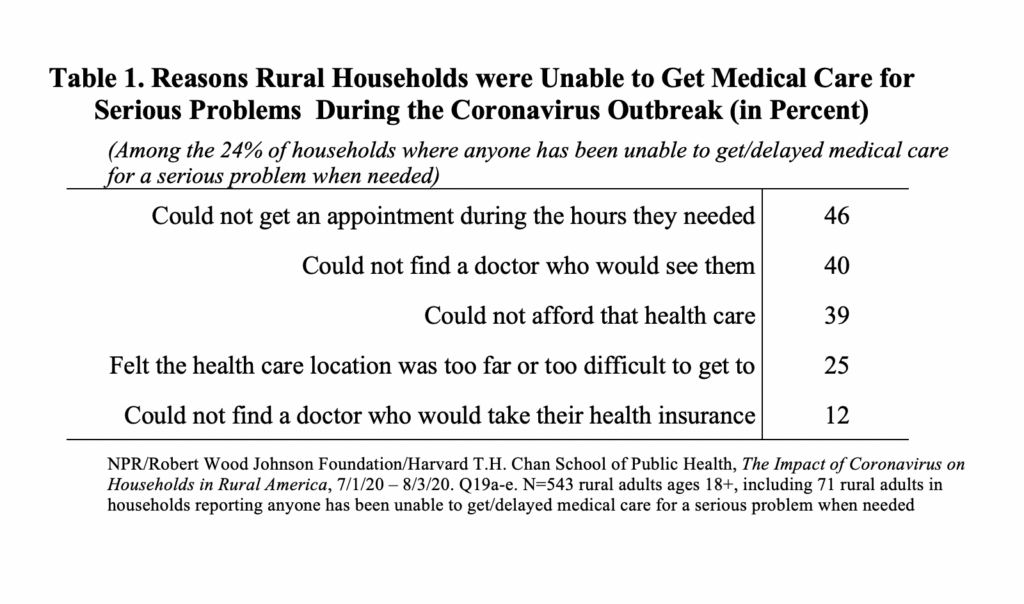
When given a list of potential reasons for not getting care, 46% of rural households report they could not get an appointment during the hours they needed, 40% report they could not find a doctor who would see them, and 39% report they could not afford that health care. One in four (25%) report they felt the health care location was too far or too difficult to get to, while 12% report they could not find a doctor who would take their health insurance (see Table 1).
Health care delays are especially concerning among rural households with chronic illnesses or with anyone who is at high risk for developing serious illness from COVID-19 due to their age or underlying medical conditions. A majority of rural households (53%) report anyone in their household is living with a chronic illness, while 42% of rural households report living with anyone who is at high risk for developing serious illness from coronavirus due to their age or underlying medical conditions.
One in three rural households with anyone who has a chronic illness (33%) report anyone in their household has been unable to get medical care for a serious problem when they needed it during the coronavirus outbreak, with a majority of those unable to get care (60%) reporting negative health consequences as a result. Similarly, one in three rural households with anyone who is at high risk for serious illness from COVID-19 (33%) report anyone in their household has been unable to get medical care for a serious problem when they needed it during the coronavirus outbreak, with a majority of those unable to get care (61%) reporting negative health consequences as a result.
This poll, The Impact of Coronavirus on Households in Rural America, was conducted July 1 – August 3, 2020, among 3,454 U.S. adults ages 18 or older, including 543 adults living in rural areas (Metropolitan Statistical Areas (MSA) with a central city whose population is under 50,000, and counties that are not part of MSAs). Adults in this survey were asked to report on serious problems facing both themselves and others living in their households, so measures are reported as a percentage of households for all household-related questions. See the Methodology below for further details.
“In a period where access to medical care is critical for many people, it is of serious concern that so many in rural America with serious medical conditions could not be seen,” said Robert J. Blendon, co-director of the survey and Richard L. Menschel Professor of Public Health and Professor of Health Policy and Political Analysis Emeritus at Harvard T.H. Chan School of Public Health. “Unlike in other studies showing this is largely related to financial issues, in this case the COVID-19 situation created a major barrier for rural Americans to be seen by a physician or hospital. It is clear that in an epidemic, we have to find better ways to manage access to care for people who need it.”
At a time when America is largely relying on the internet for their jobs and education, about one in three rural households (34%) report either having serious problems with their internet connection to do their jobs or schoolwork, or that they do not have a high-speed internet connection at home. In this environment, 46% of rural households report using telehealth, where someone in their household has received advice or treatment from a doctor or other health care professional over the phone or through a smartphone, tablet, or computer because they could not see one in person
When it comes to their finances, 42% of rural households report facing serious financial problems during the coronavirus outbreak, across a wide range of areas, including depleting household savings and serious problems paying credit card bills and other debt. Many of these problems are concentrated among Black and Latino rural households and rural households that have experienced job or wage losses since the start of the outbreak. Serious financial problems are reported by most Black or Latino rural households (85%), compared with 36% of white rural households. And when it comes to employment problems, 43% of rural households report any adult household members have lost their jobs, been furloughed, or had wages or hours reduced since the start of the outbreak, with two-thirds of these households (66%) reporting serious financial problems.
When it comes to caring for children, 54% of rural households with children report experiencing serious problems during this time. This includes about one in three (34%) facing serious problems keeping their children’s education going. Internet connectivity is also a major issue for some during this time, as four in ten rural households with children (40%) either do not have a high-speed internet connection at home or report serious problems with their internet connection to do schoolwork or their jobs.
View the complete poll findings. 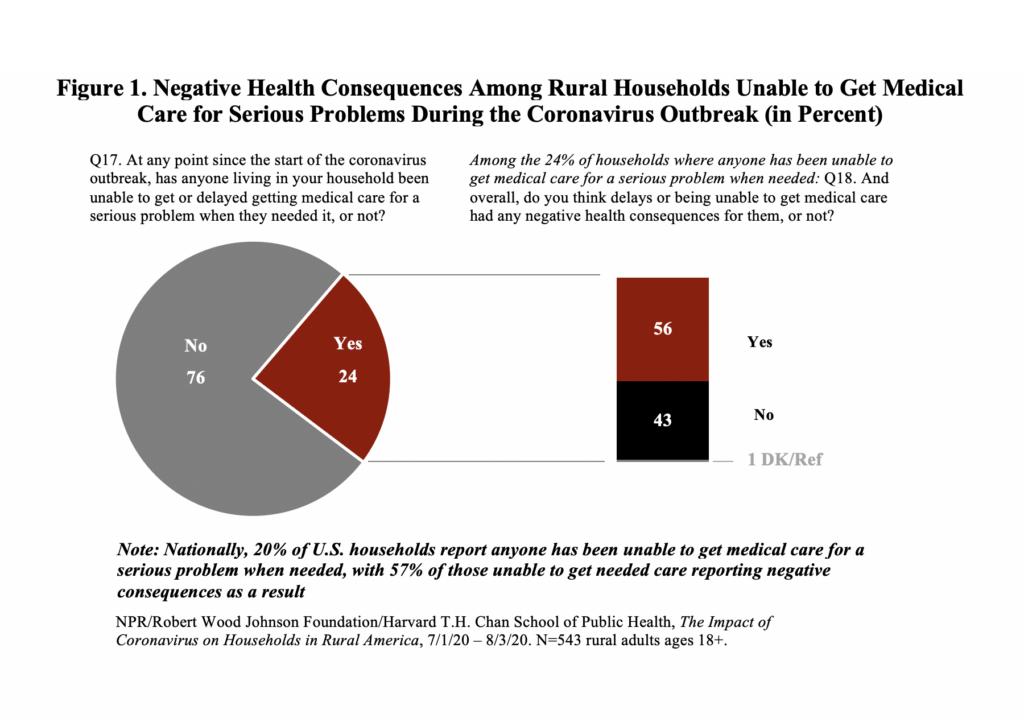
Methodology
The poll in this study is part of an on-going series of surveys developed by researchers at the Harvard Opinion Research Program (HORP) at Harvard T.H. Chan School of Public Health in partnership with the Robert Wood Johnson Foundation and NPR. The research team consists of the following members at each institution.
Harvard T.H. Chan School of Public Health: Robert J. Blendon, Professor of Public Health and Professor of Health Policy and Political Analysis Emeritus, and Executive Director of HORP; John M. Benson, Senior Research Scientist and Managing Director of HORP; Mary G. Findling, Senior Research Specialist; Chelsea Whitton Pearsall, Research Coordinator.
Robert Wood Johnson Foundation: Carolyn Miller, Senior Program Officer, Research-Evaluation-Learning; Jordan Reese, Director of Media Relations; Martina Todaro, Research Associate, Research-Evaluation-Learning.
NPR: Andrea Kissack, Senior Supervising Editor, Science Desk; Joe Neel, Deputy Senior Supervising Editor, Science Desk; Scott Hensley, Senior Editor, Science Desk.
Interviews were conducted online and via telephone (cellphone and landline), July 1 – August 3, 2020, among a nationally representative, probability-based sample of 3,454 adults age 18 or older in the U.S., including 543 adults living in rural areas. Data collection was conducted in English and Spanish by SSRS (Glen Mills, PA), an independent research company. The margin of sampling error, including the design effect, was ±3.3 percentage points nationally and ±5.4 percentage points for rural households at the 95% confidence level. In this survey, rural was defined as a Metropolitan Statistical Area (MSA) with a central city whose population is under 50,000, and counties that are not part of an MSA.
The core of the sample was address-based, with respondents sampled from the United States Postal Service’s Computerized Delivery Sequence (CDS) file. Sampled households were sent an invitation letter including a link to complete the survey online and a toll-free number that respondents could call to complete the survey with a telephone interviewer. All respondents were sent a reminder postcard, which also included a QR code they could scan to be linked to the survey via a smart device. Households that could be matched to telephone numbers and that had not yet completed the survey were called to attempt to complete an interview. In order to represent the hardest-to-reach populations, the address-based sample (ABS) was supplemented by telephone interviews with respondents who had previously completed interviews on the weekly random-digit dialing (RDD) SSRS Omnibus poll and online using the SSRS Opinion Panel, a probability-based panel.
A total of 2,992 respondents completed the questionnaire online, 127 by calling in to complete, and 335 were completed as outbound interviews.
Possible sources of non-sampling error include non-response bias, as well as question wording and ordering effects. Non-response produces some known biases in survey-derived estimates because participation tends to vary for different subgroups of the population. To compensate for these known biases and for variations in probability of selection within and across households, the samples were weighted to match the distribution of the population based on data from the U.S. Census Bureau’s 2018 American Community Survey (ACS). Weighting parameters included: gender, age, education level, race/ethnicity, and region.
Respondents who were the only person living in a household were asked about their own experiences. Respondents who had anyone else also living in their household were asked about the experiences of anyone living in the household. Together these responses represent the experience of the household.
photo: rgaudet17/pixabay.com
Nicole Rura
Harvard T.H. Chan School of Public Health
nrura@hsph.harvard.edu
617-221-4241
###
Harvard T.H. Chan School of Public Health brings together dedicated experts from many disciplines to educate new generations of global health leaders and produce powerful ideas that improve the lives and health of people everywhere. As a community of leading scientists, educators, and students, we work together to take innovative ideas from the laboratory to people’s lives—not only making scientific breakthroughs, but also working to change individual behaviors, public policies, and health care practices. Each year, more than 400 faculty members at Harvard Chan teach 1,000-plus full-time students from around the world and train thousands more through online and executive education courses. Founded in 1913 as the Harvard-MIT School of Health Officers, the School is recognized as America’s oldest professional training program in public health.
For more than 40 years the Robert Wood Johnson Foundation has worked to improve health and health care. We are working with others to build a national Culture of Health enabling everyone in America to live longer, healthier lives. For more information, visit www.rwjf.org. Follow the Foundation on Twitter at www.rwjf.org/twitter or on Facebook at www.rwjf.org/facebook.
NPR connects to audiences on the air, online, and in person. More than 26 million radio listeners tune in to NPR each week and more than 30 million unique visitors access NPR.org each month, making NPR one of the most trusted sources of news and insights on life and the arts. NPR shares compelling stories, audio and photos with millions of social media users on Facebook, Twitter, Instagram, Pinterest, YouTube and Snapchat; NPR News and NPR One apps, online streaming, podcasts, iTunes radio and connected car dashboards help meet audiences where they are. NPR’s live events bring to the stage two-way conversations between NPR hosts and the audience in collaboration with the public radio Member Station community. This robust access to public service journalism makes NPR an indispensable resource in the media landscape.
