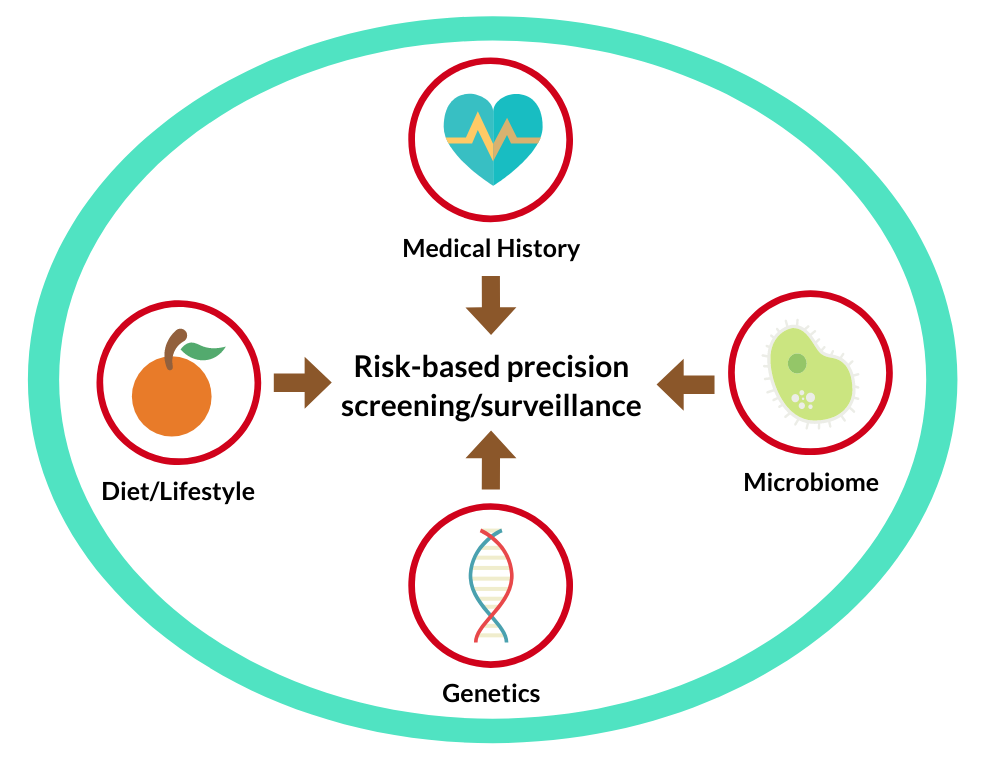
While substantial advances have been made in epidemiology to identify environmental and genetic risk factors, this knowledge has not yet been effectively translated into the clinic for better patient care. A particular example is the age-based or “one-size-fits-all” colonoscopy screening approach that does not take into account the individual variation in colorectal cancer risk. Similar issue occurs to colonoscopy surveillance after polypectomy, where histopathologic features of polyps that are being used in clinical guidelines demonstrate poor sensitivity in predicting subsequent risk of colorectal neoplasia. As a result, lower-risk patients can undergo unnecessary excess testing, whereas higher-risk patients may receive delayed or no testing. To address these gaps, our group is building a longitudinal cohort of patients who had undergone repeated colonoscopy exams in the Partners HealthCare. Detailed clinical and epidemiologic data are being extracted from the EHR systems supplemented by use of validated natural language processing algorithms; and then linked to the state cancer registry for cancer incidence and to the Partners Biobank for genomic information. Tissue specimens will be collected from the pathology departments for tumor profiling. This integrated cohort will allow us to identify novel biomarkers for early detection, validate prediction models in the real clinical setting, and develop and evaluate clinically applicable risk assessment tools for precision screening and surveillance.