
- This event has passed.
2-Day Webinar on Malaria Governance, Integrated Service Delivery, Training & Capacity Building
September 28th, 2021 - September 29th, 2021
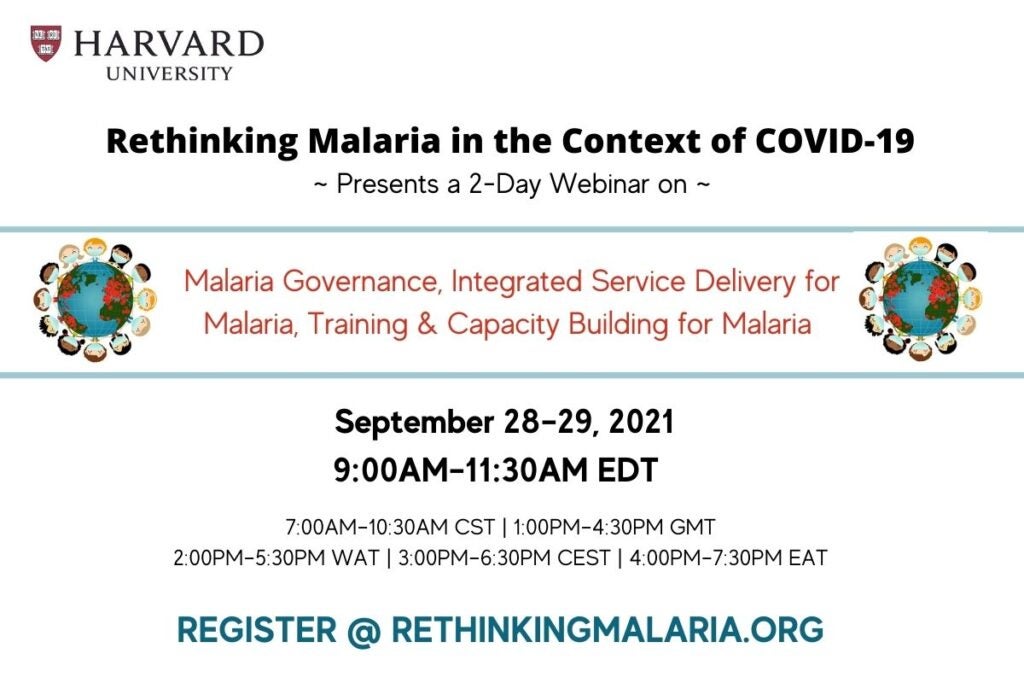
A 2-Day Participatory Webinar Discussion – “Rethinking Malaria in the Context of COVID–19”
In keeping with a longstanding academic tradition, multidisciplinary perspectives from diverse stakeholders and discussants will be offered in a neutral environment during this 2-day, public webinar. Q&A will be available during portions of the proceedings for broader engagement.
Together, we will identify and discuss actions—including some of the ideas and findings from the yearlong “Rethinking Malaria in the Context of COVID–19” global engagement—to overcome the recent plateau in malaria progress and enable the most effective and innovative response to control and eliminate malaria worldwide.
Pre-prints of the “Rethinking Malaria in the Context of COVID–19” manuscripts will be available, but not required reading to participate in the webinar.
Free registration, agenda, and information at www.rethinkingmalaria.org.

