March 2, 2018 – If a psychiatrist meets with a patient “virtually,” through videoconferencing, can privacy be assured?
Do insurance companies reimburse for virtual visits? How would those rates compare with face-to-face visits?
What are the federal and state regulations regarding telemental health?
These are some of the questions that a team of three first-year doctor of public health (DrPH) candidates at Harvard T.H. Chan School of Public Health tackled for their field practice in January, working under the guidance of clinical teams and strategic planners at McLean Hospital in Belmont, Mass., one of the nation’s top psychiatric hospitals.
As part of its strategic planning process, McLean is seeking to better understand the burgeoning field of telemental health—the provision of mental health services leveraging technology such as videoconferencing or apps on desktops, laptops, or mobile devices. McLean wanted to learn more about the regulatory and legal environment, evolving insurance reimbursement, and best practices of health providers using technology to provide mental health across the U.S.
To do so, McLean leaders enlisted Harvard Chan students’ help. Under the DrPH program’s field immersion component, doctoral candidates have an opportunity to work on real-world health-related projects in collaboration with senior administrators at a variety of host organizations. Students participate in three field immersions during their three-year program: in small teams during January of their first year; in individual placements during the summer of their second year; and for nine months in their final year as part of the Doctoral Engagement in Leadership and Translation for Action (DELTA) capstone project, in which they work full-time with an organization with the aim of significantly impacting public health, either through policy or program change or development of strategies for future change.
DrPH students spent this past January participating in a wide range of field immersion projects both in the U.S. and abroad. For example, one student team worked in Araku Valley, India to assess a new community-based cancer screening program, and another looked at ways to build capacity for neonatal services in Vietnam’s central provinces.
Building teamwork
The Harvard Chan students who worked on the McLean project, all slated to graduate in 2020, came from diverse backgrounds and brought a range of expertise and experiences to the effort. Bryan O. Buckley worked in health care management for the past five years and was previously a manger of patient safety and quality at the Michigan Health & Hospital Association’s Keystone Center. Allen Chia En Lien, a Taiwanese doctor, worked for the government of Taiwan as a political liaison on health-related issues in South Africa. Mohd Lutfi Fadil Bin Lokman, a doctor from Malaysia, has conducted health economics research for the Malaysian Ministry of Health and heads a nonprofit that builds healthcare facilities in underserved communities.
Last fall, to prepare for the McLean project, Buckley, Lien and Lokman took a Harvard Chan course called “Enabling Teams,” taught by Kimberlyn Leary, program director of the School’s Enabling Change program and executive director of policy outreach at McLean. Leary said the course is focused on distinct dimensions of teamwork, such as how to leverage the range of skills and talents that each person brings to a team and how to resolve conflicts.
Buckley said the class was extremely helpful as he, Lien, and Lokman developed a strategy for approaching the work at the hospital—“kind of like a football game plan,” he said.
The Harvard Chan students had several conference calls with their McLean mentors in the fall, then met weekly with them in January to discuss particulars of the project, including scope, logistics, expectations, information gathering, and analysis. Much of the students’ work was conducted independently. They met with McLean-based and Boston-area healthcare professionals—experts from hospitals, insurance companies, and professional associations in psychiatry, psychology, and social work—to gather information.
In roughly a dozen hour-long interviews, the students explored how the field of telemental health is evolving, how to ensure and measure quality, especially of virtual visits, regulatory trends both in Massachusetts and across the U.S., best practices regarding insurance reimbursement, and the consumer market for telemental health.
McLean Hospital leadership, including president and psychiatrist in chief Scott L. Rauch and Catharyn Gildesgame, vice president of strategic planning and implementation (who also served as one of the students’ lead mentors), shared thoughts with the students about the hospital’s mission, values, and strategic planning efforts.
In addition to the interviews, the students conducted literature reviews and market research about telemental health. At the end of every day, they gathered to review what they’d learned.
Delivering the results
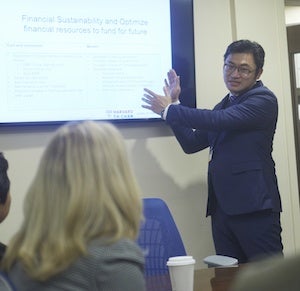
At the end of January, the students gave hospital senior leaders a 45-page report and delivered a presentation that outlined both the opportunities and challenges of telemental health. Findings included:
- Insurance reimbursements for virtual office visits may be only slightly lower than those for in-person visits.
- Videoconferencing apps like Skype or FaceTime are not secure enough to meet the requirements outlined in the Health Insurance Portability and Accountability Act of 1996 (HIPAA).
- While building or buying a secure videoconferencing system may require a substantial initial investment, conducting virtual office visits could potentially offset costs. Removing the burden of transportation from patients could help cut down on no-shows and cancellations. Virtual visits could draw new clients from places like nursing homes and correctional facilities.
- Commonwealth of Massachusetts regulations require an existing physician-patient relationship that includes taking a medical history and conducting a physical exam before e-prescribing is permissible.
Benefits all around
Members of the McLean team who had an opportunity to work with the Harvard Chan students were happy with their efforts.
Gildesgame found the students “insightful, analytic, engaging, hard-working, and collaborative.” She added, “The report and presentation that they prepared for us were thought-provoking and will inform our strategic planning going forward.”
Leary commended the students on their excellent work. “They worked effectively as a team and integrated their work with teams across the McLean ecosystem,” she said. “The field immersion also enabled them, as physicians and quality experts, to appreciate the specific challenges and opportunities of enhancing population health by underscoring how mental health is part of all health.”
For the students’ part, the experience at McLean was enlightening. Lokman and Lien said the field practice helped educate them about the workings of the U.S. health care system.
Buckley gained valuable insight from meeting with healthcare leaders at McLean and beyond. “We had the great opportunity to see how leading healthcare organizations do their work, how they strategically plan, and what their challenges are,” he said. “We learned about costs and margins and learned about the importance of proposing a business plan that’s not just a great idea, but financially sustainable.”
photos: Kent Dayton
Harvard Chan School’s DrPH professional degree program prepares students for an accelerated career path towards significant leadership roles of high impact at local, national, and international levels, in public health and healthcare. Learn more
