Patient perceptions vary significantly across seven states and nation
For immediate release: Monday, February 29, 2016
Boston, MA ─ A new NPR / Robert Wood Johnson Foundation / Harvard T.H. Chan School of Public Health poll finds that although a majority of Americans are satisfied with the health care they receive, many still experience significant problems with health care costs, insurance coverage, and accessing care when they need it.
While a strong majority of adults reflect positively on their health insurance coverage, with 33% rating theirs as “excellent” and 41% as “good,” one in four Americans rates their insurance as just fair (20%) or poor (5%). More than a quarter of adults in the U.S. also say health care costs have caused serious financial problems for them or their family. Experiences among patients differ by state of residence, but as many as one in five adults in some states say they could not get the health care they needed at some point in the past two years.
The poll surveyed more than 1,000 adults nationwide and more than 1,000 adults in each of seven states — Florida, Kansas, New Jersey, Ohio, Oregon, Texas, and Wisconsin — about their personal health care experiences and perceptions of the state in which they live. Those seven states were selected to represent a geographically diverse group of states that have and have not expanded Medicaid, as well as the only state in the nation that did not have to, as Wisconsin’s pre-ACA health insurance coverage levels already matched or exceeded those passed by health reform. Polling was conducted during the fall of 2015, after an additional estimated 17.6 million people acquired health insurance[1] in the United States.
View the report/topline
While Three in Four Adults Have a Regular Health Care Provider, One in Seven Faces Major Barriers to Accessing Health Care
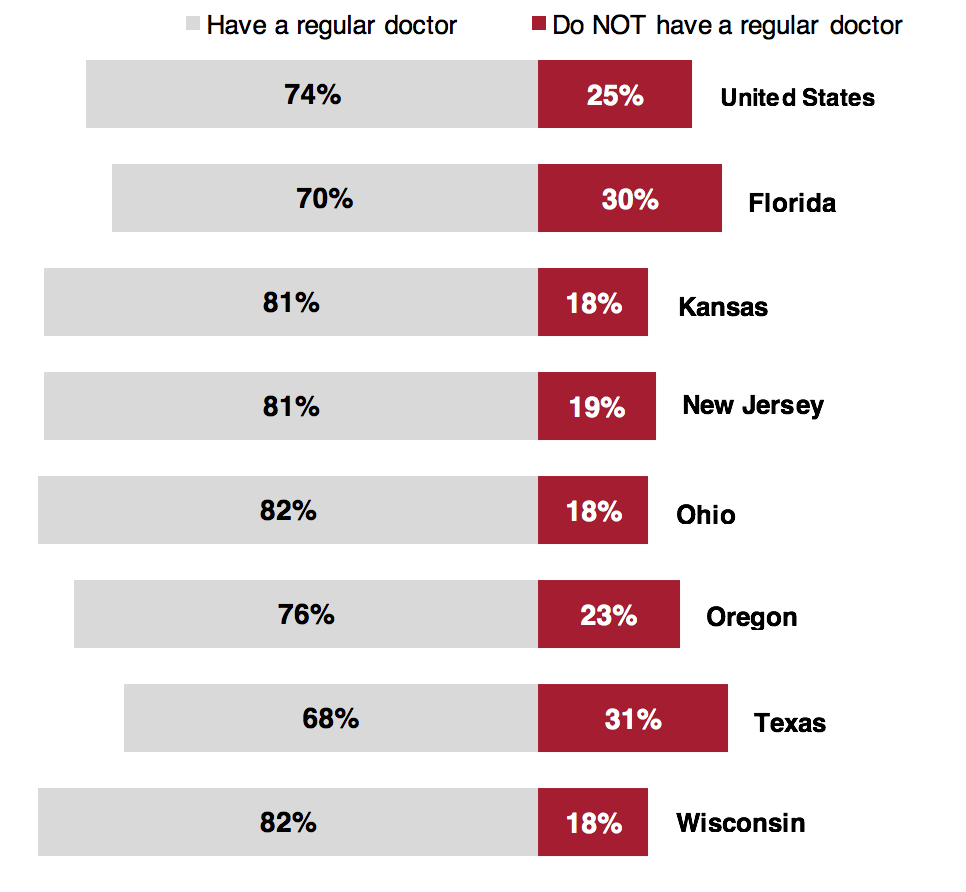
Nearly three in four (74%) Americans say they have a regular doctor or health care professional that provides most of their health care when they are sick or have a health concern; however, one in four (25%) adults in the U.S. does not. When it comes to receiving needed health care, more than one in seven (15%) adults in the U.S. say there has been at least one time in the past two years when they needed health care but could not get it. This may partially explain why one-third (33%) of adults nationwide say they have received health care in the emergency room (ER) of a hospital at least once in the past two years and why 23% of recent patients say they use the ER more now than they used to. Among those who have used the emergency room in the past two years, nearly half (47%) say they went to the ER because other facilities were not open or they could not get an appointment, they felt the ER was the only place that would treat them, or because other facilities were too far away.
Percent of adults in the U.S. who say they do or do not have a regular doctor that provides most of their care when they are sick or have a health concern:
Perceived Health Care Quality Varies Substantially by Facility
Nearly 80 percent of Americans reflect positively on the health care they personally receive, but only a third (33%) says their care is excellent, while 46 percent rate it as good. When added to the 18 percent of adults in the U.S. who say their care is fair or poor, the data suggest the United States has a long way to go if it hopes to have one of the highest-quality health care systems in the world.
The poll asked American adults who had used doctor’s offices, hospitals, emergency rooms, urgent care centers, and retail or drug store mini-clinics at least once in the past two years to rate their experiences as either excellent, good, fair, or poor. Doctor’s offices received the highest ratings, with 43 percent of patients saying the quality of their last visit was excellent, while one in eight (13%) say it was fair or poor. On the other hand, emergency rooms received the lowest ratings, with more than one in four (27%) recent patients saying the quality of their care was fair or poor.
When asked to rate six aspects of their most recent visit to a doctor, patients nationwide were most dissatisfied with their ability to get in touch with the doctor outside of an appointment by phone or email — 29% saying it was fair or poor. They were most satisfied with the doctor’s sensitivity to their cultural background — with 11% saying it was fair or poor.
Six in Ten Consider Health Care Costs Reasonable, But Many Americans Still Struggle
Sixty percent of Americans say the overall cost they personally pay for their health care, including premiums, deductibles, co-payments and prescription drugs, is reasonable; however, nearly three in ten (29%) adults in the U.S. disagree, saying the cost they personally pay for their care is unreasonable. More than a third (34%) of Americans also believes the cost of health care services has become less affordable in the past two years, and more than one in five (22%) say the same of prescription drugs.
For many Americans, rising health care costs have major financial consequences. More than one in four (26%) adults in the U.S. say health care costs have caused serious financial problems for them or their family in the past two years. Among those who say they have experienced serious problems, more than 40 percent say they have spent all or most of their personal savings on large medical bills.
“It is clear from the poll that health care costs should top the agenda for what needs to be done in the future — especially in some states, where more than a third of people have serious problems paying their bills,” said Robert J. Blendon, Richard L. Menschel Professor of Health Policy and Political Analysis at Harvard T.H. Chan School of Public Health.
Percent of adults in the U.S. who say their health care costs have or have not caused a problem for them or their family’s overall financial situation 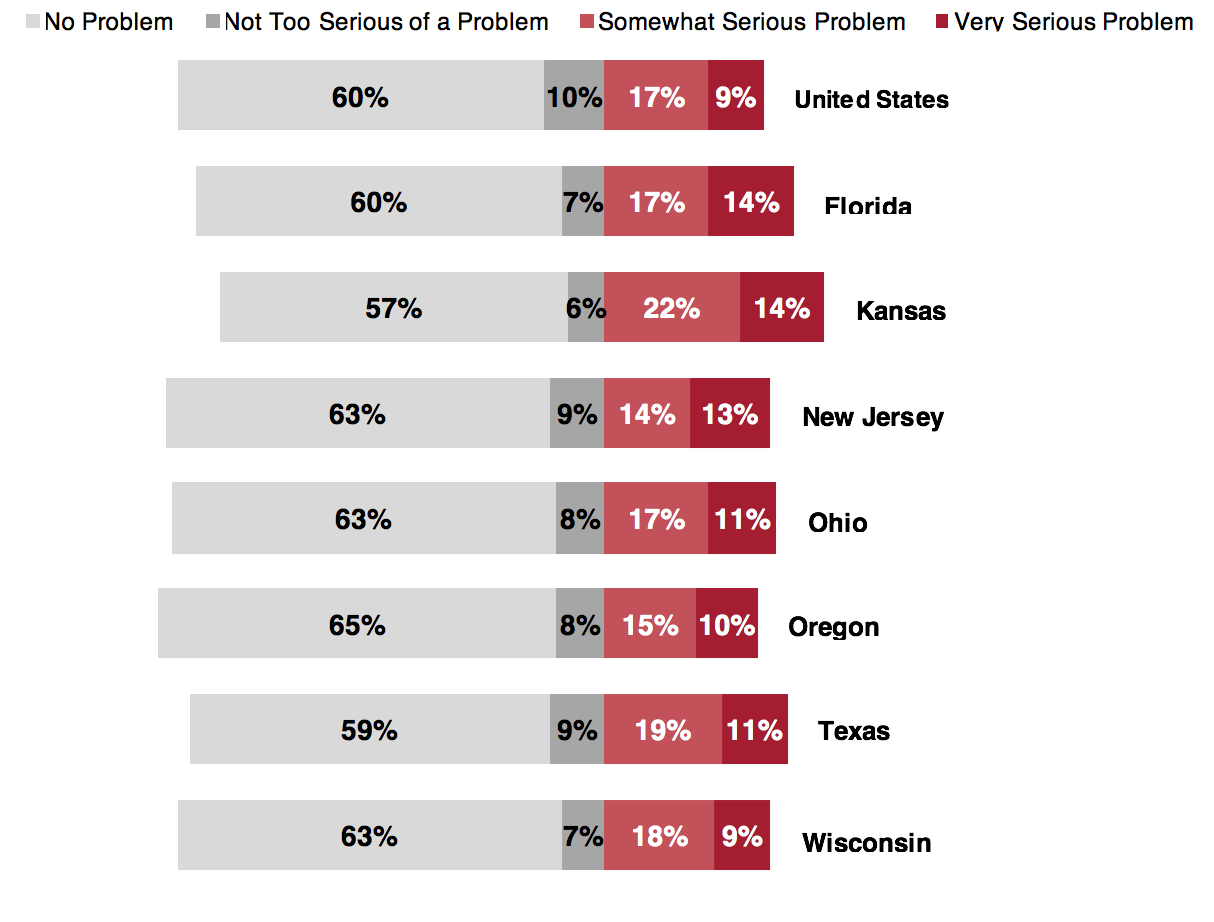
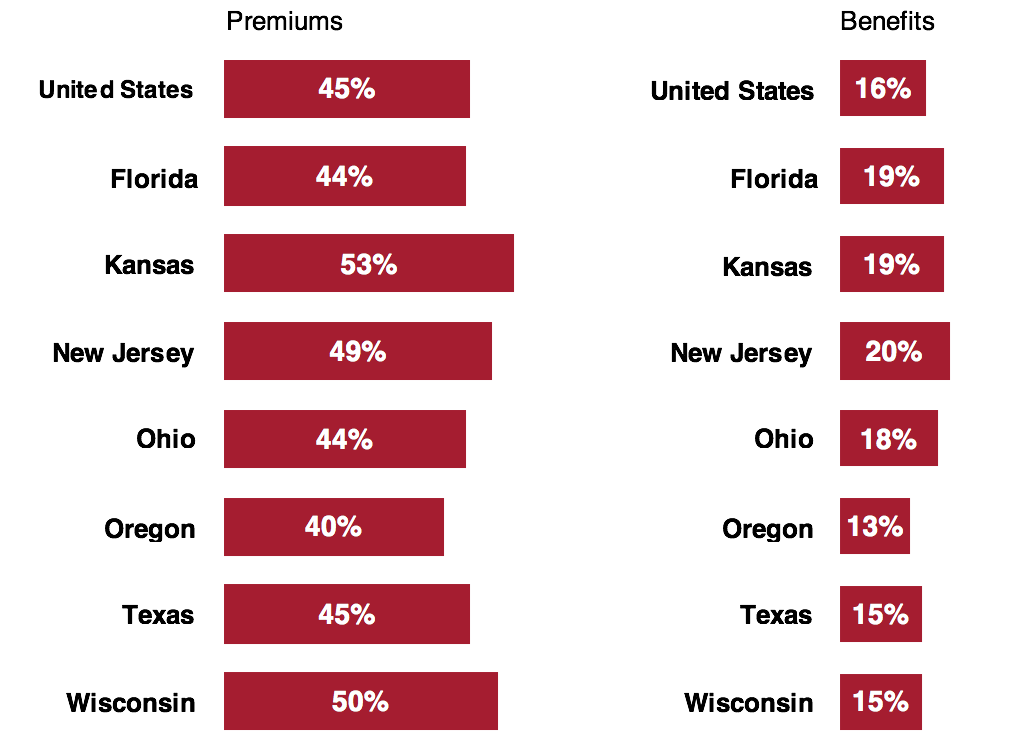
Majority of Americans Say Health Benefits Remain the Same, But Significant Numbers Say Costs Have Increased
Seventy percent of Americans with health insurance say their benefits have stayed about the same over the past two years, whereas 45% say their premiums have increased, and 35% say their co-pays and deductibles have increased. Among those who believe their benefits have changed, about the same proportion believes their benefits have decreased as increased. Overall, even though most (73%) Americans say their health insurance coverage is excellent or good, one in four (25%) adults in the U.S. says their coverage is either fair or poor.
Percent of adults in the U.S. who say their health insurance premiums or benefits have increased in the past two years
This poll is part of an ongoing series of surveys developed by researchers at the Harvard Opinion Research Program (HORP) at Harvard T.H. Chan School of Public Health in partnership with the Robert Wood Johnson Foundation and NPR. The research team consists of the following members at each institution.
Harvard T.H. Chan School of Public Health: Robert J. Blendon, Richard L. Menschel Professor of Health Policy and Political Analysis and Executive Director of HORP; John M. Benson, Research Scientist and Managing Director of HORP; Caitlin L. McMurtry, Research Assistant; and Justin M. Sayde, Administrative and Research Manager.
Robert Wood Johnson Foundation: Fred Mann, Vice President, Communications; Carolyn Miller, Senior Program Officer, Research-Evaluation-Learning; and Joe Costello, Director, Marketing.
NPR: Anne Gudenkauf, Senior Supervising Editor, Science Desk; and Joe Neel, Deputy Senior Supervising Editor, Science Desk.
The “Patients’ Perspectives on Health Care in the United States” project consisted of eight polls, conducted via telephone (including both landline and cell phone) by SSRS of Media (PA). Interviews were conducted in English and Spanish, using random-digit dialing, September 8 – November 9, 2015, among representative samples of adults age 18 or older nationally and in the seven states.
For the national poll, interviews were conducted with a nationally representative probability sample of 1,002 U.S. adults. The margin of error for total U.S. respondents is ± 3.8 percentage points at the 95% confidence level. For the state polls, sample sizes and margins of error are included in the table below:
| State | Number of Interviews | Margin of Error (percentage points) |
| Florida | 1,003 | ±3.9 |
| Kansas | 1,005 | ±3.8 |
| New Jersey | 1,003 | ±4.0 |
| Ohio | 1,000 | ±3.8 |
| Oregon | 1,009 | ±4.0 |
| Texas | 1,005 | ±3.9 |
| Wisconsin | 1,011 | ±3.9 |
Possible sources of non-sampling error include non-response bias, as well as question wording and ordering effects. Non-response in telephone surveys produces some known biases in survey-derived estimates because participation tends to vary for different subgroups of the population. To compensate for these known biases and for variations in probability of selection within and across households, sample data are weighted by household size, cell phone/landline use, and demographics (sex, age, race/ethnicity, education, marital status, and census region) to reflect the true population. Other techniques, including random-digit dialing, replicate subsamples, and systematic respondent selection within households, are used to ensure that the sample is representative.
For more information:
Marge Dwyer
617.432.8416
mhdwyer@hsph.harvard.edu
###
Harvard T.H. Chan School of Public Health brings together dedicated experts from many disciplines to educate new generations of global health leaders and produce powerful ideas that improve the lives and health of people everywhere. As a community of leading scientists, educators, and students, we work together to take innovative ideas from the laboratory to people’s lives — not only making scientific breakthroughs, but also working to change individual behaviors, public policies, and health care practices. Each year, more than 400 faculty members at Harvard Chan teach 1,000-plus full-time students from around the world and train thousands more through online and executive education courses. Founded in 1913 as the Harvard-MIT School of Health Officers, the School is recognized as America’s oldest professional training program in public health.
For more than 40 years the Robert Wood Johnson Foundation has worked to improve health and health care. We are working with others to build a national Culture of Health enabling everyone in America to live longer, healthier lives. For more information, visit www.rwjf.org. Follow the Foundation on Twitter at www.rwjf.org/twitter or on Facebook at www.rwjf.org/facebook.
NPR is the leading provider of non-commercial news and entertainment programming in the U.S. More than 27 million people listen to NPR programs each week via 800+ radio stations throughout the country. In partnership with Member Stations, NPR strives to create a more informed public – one challenged and invigorated by a deeper understanding and appreciation of events, ideas, and cultures. As a digital innovator, and a leader in the public media community, NPR assures that the unique mission of nonprofit public media is not only preserved, but grows.
[1] ObamaCare Facts, “ObamaCare Enrollment Numbers,” http://obamacarefacts.com/sign-ups/obamacare-enrollment-numbers/