Extended Cost-Effectiveness Analysis (ECEA) is a form of quantitative economic analysis that assesses the health and financial impact of health policies. It is an expansion of cost-effectiveness analysis, which compares the relative costs and gains in health outcomes (in the form of years of life saved, premature deaths averted, quality- or disability-adjusted life years gained/averted, etc.) of interventions. ECEA also includes non-health benefits such as financial risk protection and distributional consequences like equity in the economic evaluation of health policies. This enables health policy makers to take into account multiple criteria and make trade-offs among competing demands (see Figure 1).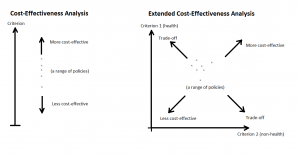
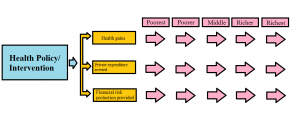
Figure 1. Cost-Effectiveness Analysis and Extended Cost-Effectiveness Analysis
The fundamental aim of health policies is to improve health outcomes (e.g. reduction in premature mortality and morbidity) at the population level. However, health policies can provide other benefits, extending to other sectors than the sole health sector. An important non-health benefit of such policies is the provision of financial risk protection (FRP), or the reduction of individuals’ and households’ impoverishment; in addition to improved health equity among the population by providing progressive redistribution of the health benefits and impoverishment averted (see Figure 2).
Figure 2. Basic structure of Extended Cost-Effectiveness Analysis
ECEA presents the assessment of health policy in three domains: 1) health gains, 2) private expenditures averted, and 3) FRP; all per population subgroup (e.g. income quintile, geographical setting). Additionally, with the total costs of the policy assessed, we can calculate the outcomes of health gains and financial protection per dollar expenditure. In this respect, using ECEA, every policy/intervention can be placed in a two-dimensional space by 1) health benefits per dollar expenditure and 2) FRP per dollar expenditure (Figure 1). Policy makers can then visually compare different policies/interventions, taking into account multiple criteria in the decision-making process.
More broadly, the added dimension of assessment outside of the health sector is not limited to financial benefits, but could also include educational, agricultural, environmental benefits, to name a few. ECEA not only can assess the equity between different income quintiles, but also the disaggregation of any type, geographically and demographically.
Below is a selection of recently published ECEA studies:
| Topic | Policy instrument | Country | Publication(s) |
| Expanding surgical access | Task sharing, public finance | Ethiopia | [2] |
| Home-based neonatal care package | Public finance | India | [3,4] |
| Diarrhea and pneumonia treatment | Public finance | Ethiopia | [5-8] |
| Human papillomavirus vaccination to prevent cervical cancer | Public finance | China | [9] |
| Universal coverage for mental, neurological, and substance use disorders | Public finance | Ethiopia, India | [10-13] |
| Selected ECEAs for cardiovascular diseases | Public finance of interventions, tobacco taxation, regulation of salt | China, Ethiopia, South Africa | [14-16] |
| Motorcycle helmet laws | Regulation | Vietnam | [17] |
| Use of liquefied petroleum gas and other clean energy sources in household | Commodity subsidy | India | [18] |
| Postponing adolescent parity | Education | India, Niger | [19] |
| Tuberculosis treatment | Universal public finance; policies to improve ease of borrowing for treatment costs | India | [20] |
| Measles vaccine | Conditional cash transfers | Ethiopia | [21] |
| Universal immunization | Public finance | India | [22] |
| Water and sanitation | Clean piped water and improved sanitation | India | [23] |
| Tobacco | Taxation | China, Lebanon, Armenia | [16, 24-25] |
| Rotavirus vaccine | Public finance | India, Ethiopia, Malaysia | [5,26] |
*This list is adapted from: Verguet and Jamison. 2018. Chapter 8. Health policy analysis: applications of extended cost-effectiveness analysis (ECEA) methodology in DCP3. In: Jamison DT, Nugent R, Gelband H, Horton S, Jha P, Laxminarayan R, eds. Disease Control Priorities. Volume 9: Disease control priorities, improving health and reducing poverty. Washington, DC: World Bank 2018.
References
- Verguet, S., Kim, J.J. and Jamison, D.T., 2016. Extended cost-effectiveness analysis for health policy assessment: a tutorial. Pharmacoeconomics, 34(9), pp.913-923. https://link.springer.com/article/10.1007/s40273-016-0414-z
- Shrime, M.G., Verguet, S., Johansson, K.A., Desalegn, D., Jamison, D.T. and Kruk, M.E., 2015. Task-sharing or public finance for the expansion of surgical access in rural Ethiopia: an extended cost-effectiveness analysis. Health policy and planning, 31(6), pp.706-716. https://academic.oup.com/heapol/article/31/6/706/1749643/Task-sharing-or-public-finance-for-the-expansion
- Ashok, A., Nandi, A., and Laxminarayan, R. (2016). The Benefits of a Universal Home-Based Neonatal Care Package in Rural India: An Extended Cost-Effectiveness Analysis. In Disease Control Priorities, Third Edition (Volume 2): Reproductive, Maternal, Newborn, and Child Health, pg 335 – 344. https://elibrary.worldbank.org/doi/abs/10.1596/978-1-4648-0348-2_ch18
- Nandi, A., Colson, A.R., Verma, A., Megiddo, I., Ashok, A. and Laxminarayan, R., 2015. Health and economic benefits of scaling up a home-based neonatal care package in rural India: a modelling analysis. Health policy and planning, 31(5), pp.634-644. https://academic.oup.com/heapol/article/31/5/634/2355739/Health-and-economic-benefits-of-scaling-up-a-home
- Verguet, S., Murphy, S., Anderson, B., Johansson, K.A., Glass, R. and Rheingans, R., 2013. Public finance of rotavirus vaccination in India and Ethiopia: an extended cost-effectiveness analysis. Vaccine, 31(42), pp.4902-4910. http://www.sciencedirect.com/science/article/pii/S0264410X13009389
- Johansson, K.A., Memirie, S.T., Pecenka, C., Jamison, D.T. and Verguet, S., 2015. Health gains and financial protection from pneumococcal vaccination and pneumonia treatment in Ethiopia: results from an extended cost-effectiveness analysis. PloS one, 10(12), p.e0142691. http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0142691
- Pecenka, C.J., Johansson, K.A., Memirie, S.T., Jamison, D.T. and Verguet, S., 2015. Health gains and financial risk protection: an extended cost-effectiveness analysis of treatment and prevention of diarrhoea in Ethiopia. BMJ open, 5(4), p.e006402. http://bmjopen.bmj.com/content/5/4/e006402
- Verguet, S., Pecenka, C., Johansson, K.A., Memirie, S.T., Friberg, I.K., Driessen, J.R. and Jamison, D.T., 2016. Health Gains and Financial Risk Protection Afforded by Treatment and Prevention of Diarrhea and Pneumonia in Ethiopia: An Extended Cost-Effectiveness Analysis. Reproductive, Maternal, Newborn, and Child Health. In Disease Control Priorities (third edition): Volume 2, Reproductive, Maternal, Newborn, and Child Health, edited by R. Black, R. Laxminarayan, M. Temmerman, and N. Walker. Washington, DC: World Bank. https://www.ncbi.nlm.nih.gov/books/NBK361923/
- Levin, C.E., Sharma, M., Olson, Z., Verguet, S., Shi, J.F., Wang, S.M., Qiao, Y.L., Jamison, D.T. and Kim, J.J., 2015. An extended cost-effectiveness analysis of publicly financed HPV vaccination to prevent cervical cancer in China. Vaccine, 33(24), pp.2830-2841. http://www.sciencedirect.com/science/article/pii/S0264410X15002418
- Chisholm, D., Johansson, K.A., Reykar, N., Megiddo, I., Nigam, A., Strand, K.B., Colson, A., Fekadu, A. and Verguet, S., 2016. Universal health coverage for mental, neurological, and substance use disorders: an extended cost-effectiveness analysis. In Disease Control Priorities (third edition): Volume 4, Mental, Neurological, and Substance Use Disorders, edited by V. Patel, D. Chisholm, T. Dua, R. Laxminarayan, and M. Medina-Mora. Washington, DC: World Bank. https://www.ncbi.nlm.nih.gov/books/NBK361946/
- Johansson, K.A., Strand, K.B., Fekadu, A. and Chisholm, D., 2016. Health Gains and Financial Protection Provided by the Ethiopian Mental Health Strategy: an Extended Cost-Effectiveness Analysis. Health policy and planning, 32(3), pp.376-383. https://academic.oup.com/heapol/article/2907867
- Megiddo, I., Colson, A., Chisholm, D., Dua, T., Nandi, A. and Laxminarayan, R., 2016. Health and economic benefits of public financing of epilepsy treatment in India: An agent‐based simulation model. Epilepsia, 57(3), pp.464-474. http://onlinelibrary.wiley.com/doi/10.1111/epi.13294/full
- Raykar, N., Nigam, A. and Chisholm, D., 2016. An extended cost-effectiveness analysis of schizophrenia treatment in India under universal public finance. Cost Effectiveness and Resource Allocation, 14(1), p.9. https://resource-allocation.biomedcentral.com/articles/10.1186/s12962-016-0058-z
- Watkins, D.A., Olson, Z.D., Verguet, S., Nugent, R.A. and Jamison, D.T., 2015. Cardiovascular disease and impoverishment averted due to a salt reduction policy in South Africa: an extended cost-effectiveness analysis. Health policy and planning, 31(1), pp.75-82. https://academic.oup.com/heapol/article/31/1/75/2363529
- Verguet, S., Olson, Z.D., Babigumira, J.B., Desalegn, D., Johansson, K.A., Kruk, M.E., Levin, C.E., Nugent, R.A., Pecenka, C., Shrime, M.G. and Memirie, S.T., 2015. Health gains and financial risk protection afforded by public financing of selected interventions in Ethiopia: an extended cost-effectiveness analysis. The Lancet Global Health, 3(5), pp.e288-e296. http://www.sciencedirect.com/science/article/pii/S2214109X14703468
- Verguet, S., Gauvreau, C.L., Mishra, S., MacLennan, M., Murphy, S.M., Brouwer, E.D., Nugent, R.A., Zhao, K., Jha, P. and Jamison, D.T., 2015. The consequences of tobacco tax on household health and finances in rich and poor smokers in China: an extended cost-effectiveness analysis. The Lancet Global Health, 3(4), pp.e206-e216. http://www.sciencedirect.com/science/article/pii/S2214109X15700951
- Olson, Z., Staples, J.A., Mock, C., Nguyen, N.P., Bachani, A.M., Nugent, R. and Verguet, S., 2016. Helmet regulation in Vietnam: impact on health, equity and medical impoverishment. Injury prevention, 22(4), pp.233-238. http://injuryprevention.bmj.com/content/22/4/233
- Pillarisetti, A., Jamison, D.T. and Smith, K.R., 2017. Household Energy Interventions and Health and Finances in Haryana, India: An Extended Cost-Effectiveness Analysis. In Disease Control Priorities (third edition): Volume 7, Injury Prevention and Environmental Health, edited by C. N. Mock, O. Kobusingye, R. Nugent, and K. R. Smith. Washington, DC: World Bank. http://dcp-3.org/node/2506
- Verguet, S., Nandi, A., Filippi, V. and Bundy, D.A., 2016. Maternal-related deaths and impoverishment among adolescent girls in India and Niger: findings from a modelling study. BMJ open, 6(9), p.e011586. http://bmjopen.bmj.com/content/6/9/e011586
- Verguet, S., Laxminarayan, R. and Jamison, D.T., 2015. Universal public Finance of tuberculosis treatment in India: an extended cost‐effectiveness analysis. Health economics, 24(3), pp.318-332. http://onlinelibrary.wiley.com/doi/10.1002/hec.3019/full
- Driessen, J., Olson, Z.D., Jamison, D.T. and Verguet, S., 2015. Comparing the health and social protection effects of measles vaccination strategies in Ethiopia: An extended cost-effectiveness analysis. Social Science & Medicine, 139, pp.115-122. http://www.sciencedirect.com/science/article/pii/S0277953615003500
- Megiddo, I., Colson, A., Chisholm, D., Dua, T., Nandi, A. and Laxminarayan, R., 2016. Health and economic benefits of public financing of epilepsy treatment in India: An agent‐based simulation model. Epilepsia, 57(3), pp.464-474. http://onlinelibrary.wiley.com/doi/10.1111/epi.13294/full
- Nandi, A., Megiddo, I., Ashok, A., Verma, A. and Laxminarayan, R., 2017. Reduced burden of childhood diarrheal diseases through increased access to water and sanitation in India: A modeling analysis. Social Science & Medicine, 180, pp.181-192. http://www.sciencedirect.com/science/article/pii/S0277953616304853
- Salti, N., Brouwer, E. and Verguet, S., 2016. The health, financial and distributional consequences of increases in the tobacco excise tax among smokers in Lebanon. Social Science & Medicine, 170, pp.161-169. http://www.sciencedirect.com/science/article/pii/S0277953616305883
- Postolovska, I., Lavado, R.F., Tarr, G. and Verguet, S., 2017. Estimating the Distributional Impact of Increasing Taxes on Tobacco Products in Armenia. http://documents.worldbank.org/curated/en/604501492414938391/Estimating-the-distributional-impact-of-increasing-taxes-on-tobacco-products-in-Armenia-results-from-an-extended-cost-effectiveness-analysis
- Loganathan, T., Jit, M., Hutubessy, R., Ng, C.W., Lee, W.S. and Verguet, S., 2016. Rotavirus vaccines contribute towards universal health coverage in a mixed public–private healthcare system. Tropical medicine & international health, 21(11), pp.1458-1467. http://onlinelibrary.wiley.com/doi/10.1111/tmi.12766/full