Making visible the invisible: A new tool for US health departments to monitor – and boost efforts to address – socioeconomic inequalities in health
The problem: scant socioeconomic data in US public health surveillance systems
Social inequality kills. It unduly deprives individuals and communities experiencing social deprivation of their health, increases their burden of disability and disease, and cuts short their lives . Recognizing the powerful toll of social inequality on health and well-being, the objectives of Healthy People 2010 seek “to achieve two overarching goals
“:
- Increase quality and years of healthy life
- Eliminate health disparities
At issue are “health disparities among segments of the population, including differences that occur by gender, race or ethnicity, education or income, disability, geographic location, or sexual orientation .”
Yet, despite widespread recognition of the toll of economic deprivation on health, in the US we face a critical problem hampering public health departments’ ability to mobilize public concern and resources to eliminate socioeconomic inequalities in health. Why?
The problem is a lack of routine community-based data on the magnitude and trends of socioeconomic inequalities in health, due to the lack of socioeconomic data in most US public health surveillance systems, other than birth and death . Although specialized surveys, such as the National Health Interview Survey and the Behavioral Risk Factor Surveillance System do collect socioeconomic data, the vast majority of “disease- and condition-specific surveillance systems and administrative data systems do not collect such data
.” The net effect is to obscure socioeconomic gradients in health and the contribution of economic deprivation to racial/ethnic and gender inequalities in health, at the national, state, and local level
.
Rendered invisible, these preventable disparities in health remain hidden to the view of the public and policy-makers alike. The old adage applies: “if you don’t ask, you don’t know, and if you don’t know, you can’t act.” Inertia and fatalism flourish, with anecdotal knowledge about “the poor are always sicker and always with us” unchallenged by evidence that the patterning of socioeconomic inequalities in health varies by time and place and hence is not an immutable or unalterable “fact” beyond the reach of concerted effort to change
.
The absence of state and local public health surveillance data on socioeconomic inequalities in health has national ramifications. Reflecting the absence of these data, the federal report Health United States 2002 , lacked socioeconomic data in 85% of its 71 tables on “Health Status and Determinants;” virtually all of these tables, however, were stratified by “sex, race, and Hispanic origin.” Similarly, fully 70% of the 467 U.S. Healthy People 2010 objectives have no socioeconomic targets, given a lack of baseline data
. As a nation, we cannot assess whether socioeconomic inequalities are diminishing or growing over time, or if patterns vary by region or state, or by racial/ethnic-gender group, within and across diverse outcomes.
Why does this matter? Because health statistics accurately depicting the population burden of disease, disability and death, as cogently stated in the new federal report Shaping a Health Statistics Vision for the 21st century , “fulfill essential functions for public health, the health services system, and our society”. They help us understand “where we stand in terms of health as individuals, as subgroups, and as a society,” including with regard to “the existence of health disparities
.”
Additionally,
“Health statistics provide us with the information upon which we can base important public decisions at the local, state, and national levels. Once we have made those public decisions, health statistics make us accountable for the decisions that we have made. Health statistics thus enable us to evaluate the impact of health policies and health programs on the public’s health. In short, health statistics give us the information we need to improve the population’s health and to reduce health disparities
”.
Indeed, the critical importance of documenting the social patterning of disease and death has been recognized since the rise of the public health movement in the mid-19th century14 and is of national and global significance . As Edgar Sydenstricker noted, when establishing the first US population-based morbidity studies in the 1920s, these data are crucial to “give glimpses of what the sanitarian has long wanted to see – a picture of the public-health situation as a whole, drawn in proper perspective and painted in true colors
.” It was similarly Sydenstricker’s profound recognition of the importance of economic deprivation in shaping population health that led to his conducting, in 1935-1936, the first national, federally-sponsored 10-city study on the health impact of the Depression, forerunner to what ultimately became the National Health Interview Survey
.
Perhaps the most potent reason why it matters to document and monitor socioeconomic disparities in health is that this evidence is vital to boost efforts to reduce these disparities . In 1905, Hermann M. Biggs (1859-1923), internationally renowned for his work in the New York City Health Department and later as Commissioner of Health for New York State, roundly declared
:
“Public health is purchasable. Within natural limitations a community can determine its own death rate.”
Biggs’ central point was that societal resources, wisely invested, were key to improving population health – and that these resources could only be secured if fundamental data on population health and its determinants were widely understood and appreciated, by the general public and policy-makers alike. Absent data on the public’s health, as Biggs and other public health leaders of his generation had learned , appeals for resources and regulations to improve the public’s health – and for collaboration across different government agencies to develop and implement the necessary policies – would have no standing or clout.
In 1911, the motto “Public Health is Purchasable” became the official slogan of the Monthly Bulletin of the NYC Health Department, with the rationale solidly explained in an editorial by Biggs, reflecting the era’s language of social reform :
“Disease is a largely removable evil. It continues to afflict humanity, not only because of incomplete knowledge of its causes and lack of individual and public hygiene, but also because it is extensively fostered by harsh economic and industrial conditions and by wretched housing in congested communities. These conditions and consequently the disease which spring from them can be removed by better social organization. No duty of society, acting through its government agencies, is paramount to this obligation to attack the removable
cause of disease. The duty of leading this attack and bringing home to public opinion the fact that the community can buy its own health protection is laid upon all health officers, organization and individuals interested in public health movements. For the provision of more and better facilities for the protection of the public health must come in the last analysis through the education of public opinion so that the community shall vividly realize both its needs and its powers. The modern spirit of social religion, dealing with the concrete facts of life, demands the reduction of the death rate as the first result of its activity. The reduction of the death rate is the principal statistical expression and index of human and social progress. It means the saving and lengthening of the lives of thousands of citizens, the extension of the vigorous working period into old age, and the prevention of inefficiency, misery, and suffering. These advances can be made by organized social reform. Public health is purchasable.”
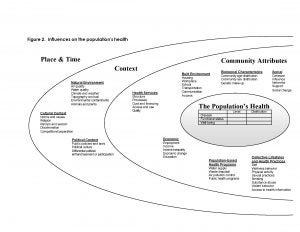
Indeed, as suggested by the population health model articulated in Shaping a Health Statistics Vision for the 21st century (Figure 1 below), it is obvious that the field of public health cannot, by itself, improve health and prevent disease; a societal effort is required. As part of this effort, however, it is our singular task—and fundamental responsibility–to provide the data on population distributions of health, disease, disability and death, and social disparities in these outcomes. Or, as stated in Healthy People 2010
:
“Healthy People 2010 recognizes that communities, States, and national organizations will need to take a multidisciplinary approach to achieving health equity—an approach that involves improving health, education, housing, labor, justice, transportation, agriculture, and the environment, as well as data collection itself. In fact, current data collection methods make it impossible to assess accurately the health status for some populations, particularly relatively small ones.”
Improvements in US health over the course of the 20th century, and especially the decline in childhood infectious disease, demonstrate the salience of Biggs’ words. So too does a burgeoning European and Canadian literature on the vital necessity of documenting social inequalities in health as an essential component of what policy makers need to take up these disparities a matter of key importance requiring intersectoral work.
Examples of population health reports emphasizing social inequalities in health that galvanized policy initiatives to address these disparities: Canada and the United Kingdom
Population health reports emphasizing social inequalities in health:
- Health Canada. Achieving Health for All: A Framework for Health Promotion (1986).
- Canada Health Canada. Population health/Santé de la Population.
- Health Canada. Toward a Healthy Future – Second Report on the Health of Canadians (1999).
- DHHS (Department of Health and Society Security). Inequalities in Health: Report of a Working Group. London: DHHS, 1980. (“The Black Report”); see also:Townsend P, Davidson N (eds). Inequalities in Health: The Black Report (3rd ed); Whitehead M. The Health Divide. London: Penguin Books, 1988.
- Drever F, Whitehead M (eds). Health Inequalities: Decennial Supplement. London: The Stationary Office, 1997.
- Acheson D, Barker D, Chambers J, Graham H, Marmot M, Whitehead M. The Report of the Independent Inquiry into Health Inequalities. London: The Stationary Office, 1998. (“The Acheson Report”)
Subsequent policy initiatives galvanized by these reports:
- Health Canada. Population Health Mobilization: A Regional Strategy – June 1999.
- Health Canada. Strategies for Population Health: Investing in the Health of Canadians. Prepared by the Federal, Provincial and Territorial Advisory Committee on Population Health for the Meeting of Ministers of Health, Halifax, Nova Scotia, Sept 14-15, 1994.
- UK Department of Health. Saving Lives: Our Healthier Nation. London: The Stationary Office, 1999.
- Department of Health. Reducing Health Inequalities: An Action Report. London: Department of Health, 1999.
- UK Department of Health. Our Healthier Nation.
A solution: geocoding and using area-based socioeconomic measures –
key findings of The Public Health Disparities Geocoding Project
Fortunately, one potential and relatively inexpensive solution to the problem of absent or limited socioeconomic data in US public health surveillance systems is provided by the methodology of geocoding residential addresses and using area-based socioeconomic measures (ABSMs) . In this approach, which draws on multilevel frameworks and area-based measures, both cases (numerators) and the catchment population (denominators) are classified by the socioeconomic characteristics of their residential area, thereby permitting calculation of rates stratified by the ABSMs.
Yet, although this approach has been employed in US health research for over 75 years (see below) , to date there exists no consensus or standard as to which ABSMs, at which level of geography, are best suited for monitoring US socioeconomic inequalities in health, whether within the total population or within diverse racial/ethnic-gender groups
. Instead, published research has exhibited a remarkable eclecticism regarding choice of geographic level and types of ABSM used, both single-variable and composite
. Although such a plurality of measures may be useful for etiologic research, in the case of monitoring, such heterogeneity impedes comparing results across studies, across outcomes, regions, and over time.
The utility of linking public health data to US census-based socioeconomic data to assess socioeconomic inequalities in health was first recognized in the 1920s and 1930s, in pathbreaking studies supported by the National Tuberculosis Association, following establishment of the first census tracts in New York City in 1906. These investigations, listed below, assessed people’s risk of TB and later other health outcomes in relationship to socioeconomic conditions of their census tracts, which initially were also termed “sanitary areas” because of their utility for public health planning.
- Nathan WB. Health conditions in North Harlem 1923-1927. New York: National Tuberculosis Association, 1932.
- Green HW. Tuberculosis and economic strata, Cleveland’s Five-City Area, 1928-1931. Cleveland, OH: Anti-Tuberculosis League, 1932.
- Green HW. The use of census tracts in analyzing the population of a metropolitan community. J Am Stat Assoc 1933; 28:147-153.
- Terris M. Relation of economic status to tuberculosis mortality by age and sex. Am J Public Health 1948; 38:1061-70.
For additional discussion of early use of census tract data in public health analyses, see:
- Watkins RJ. Introduction. In: Watkins RJ, Swift AL Jr, Green HW, Eckler AR. Golden Anniversary of Census Tracts, 1956. Washington, DC: American Statistical Association; 1956:1-2.
- Coulter EJ, Guralnick L. Analysis of vital statistics by census tract. J Am Stat Assoc 1959;54:730-40.
We accordingly launched the Public Health Disparities Geocoding Project to ascertain which ABSMs, at which geographic level (census block group [BG], census tract [CT], or ZIP Code [ZC]), would be most apt for monitoring US socioeconomic inequalities in the health. To provide a robust evaluation, guided by ecosocial theory , we designed the study to encompass a wide variety of health outcomes, hypothesizing that some ABSMs and geographic levels might be more sensitive to socioeconomic gradients for some health outcomes than others. Drawing on 1990 census data and public health surveillance systems of 2 New England states, Massachusetts and Rhode Island, we included 7 types of outcomes: mortality (all cause and cause-specific), cancer incidence (all-sites and site-specific), low birth weight, childhood lead poisoning, sexually transmitted infections, tuberculosis, and non-fatal weapons-related injuries
.
We likewise hypothesized that some socioeconomic measures might be more sensitive than others to socioeconomic gradients in health, and so analyzed socioeconomic gradients in relation to 18 ABSMs: 11 single-variable and 7 composite (Table 1: Area-based socioeconomic measures: constructs and operational definitions, using 1990 US census data). Pertinent a priori considerations to decide which measure(s) at which geographic level(s) would be best suited for monitoring socioeconomic gradients in health across diverse outcomes and within diverse racial/ethnic-gender groups were derived in part from Rossi and Gilmartin’s criteria for valid and useful social indicators , and included: (a) external validity (do the measures find gradients in the direction reported in the literature, i.e., positive, negative, or none, and across the full range of the distribution?), (b) robustness (do the measures detect expected gradients across a wide range of outcomes?), (c) completeness (is the measure relatively unaffected by missing data?), and (d) user-friendliness (how easy is the measure to understand and explain?).
Based on our methodologic research (see our appended published papers), our key methodologic finding was that the ABSM most apt for monitoring socioeconomic inequalities in health was the census tract (CT) poverty level . Specifically, we demonstrated that the CT poverty measure:
- consistently detected expected socioeconomic gradients in health across a wide range of health outcomes, among both the total population and diverse racial/ethnic-gender groups;
- yielded maximal geocoding and linkage to area-based socioeconomic data (compared to BG and ZC data), and
- was readily interpretable to and could feasibly be used by state health department staff
Indeed, fully 98% of our records could be geocoded to CT level, and data on poverty was missing for only 0.7% of the catchment area’s CTs. We also demonstrated that:
- accuracy of geocoding, not just completeness, matters
;
- ZIP Code data should not be used, because of biases introduced by the spatiotemporal mismatch of ZIP Code and US Census data
; and
- some socioeconomic measures (e.g., pertaining to wealth and to income inequality) were particularly insensitive to the expected socioeconomic gradients observed with the poverty measure and other ABSMs designed to measure economic deprivation.
Based on these considerations, we arrived at our recommendation that the CT level measure of “percent of persons below poverty” would be most apt for monitoring US socioeconomic inequalities in health.
In Figure 2, we show what socioeconomic gradients in health would look like, across our varied outcomes, if routinely monitored using the CT poverty measure. According to the US Census Bureau, CTs are “small, relatively permanent statistical subdivision of a county … designed to be relatively homogeneous with respect to population characteristics, economic status, and living conditions” and on average contain 4,000 persons . For 1990 census data, the poverty line (which varies by household size and age composition) equaled $12,647 for a family of 2 adults and 2 children
. In this Figure, we employ the following a priori cut points for the CT measure “percent of persons below poverty,” based on our prior analyses
: 0-4.9%, 5.0-9.9%, 10.0-19.9%, and >=20%, the federal definition of a “poverty area.
”
Using this measure, we were able to provide evidence of powerful socioeconomic gradients not only for mortality and low birthweight, as has been well documented , but also for myriad other outcomes for which socioeconomic data in the US are not routinely available: sexually transmitted infections, tuberculosis, violence, cancer incidence, and childhood lead poisoning. Additionally advantages were that:
- We were able to assess socioeconomic gradients in health, within the total population and diverse racial/ethnic-gender groups using a consistent socioeconomic measure across all outcomes, from birth to death, thereby avoiding well-known problems with individual-level measures of education and occupation (e.g., how to classify children and others who have not completed their education or who are not in the paid labor force)
.
- We could show that adjusting solely for CT poverty substantially reduced excess risk observed in the black and Hispanic compared to white population.
- We likewise could generate what to our knowledge is the first statewide data on the population attributable fraction in relation to poverty, whereby we found that for half the outcomes over 50% of cases overall would have been averted if everyone’s risk equaled that of persons in the least impoverished CT, the only group that consistently achieved Healthy People 2000 goals a decade ahead of time.
- Lastly, the approach we employed permitted documenting the temporal persistence—and worsening status of—a previously identified “zone of excess mortality.”
Equally salient, our method relied solely on appending nationally-available and widely-accessible US census data to the relevant public health records, thereby generating state-level data that could be aggregated up to national-level data, to monitor national trends in socioeconomic inequalities in health. Indeed, a recently issued monograph from the National Cancer Institute, on Area Socioeconomic Variations in U.S. Cancer , does just this: following the recommendation of our project, it employed the census-derived poverty measure at the tract level, where feasible, or otherwise at the county level, to document socioeconomic inequalities in cancer incidence, stage, treatment, survival, and mortality.
Importantly, the methodology we employed does not treat CT-level measures as a “proxy” for individual-level measures. Rather, it posits that ABSMs capture a mix of individual- and/or area-based socioeconomic effects, if extant. Likely at issue are a complex combination of 3 factors: (1) composition (people in poor areas have poor health because poor people, as individuals, have poor health), (2) context (people in poor areas also have poor health because concentration of poverty creates or exacerbates harmful social interactions), and (3) location of public goods or environmental conditions (poor areas are less likely to have good supermarkets and are more likely to be situated next to industrial plants, thereby harming health of their residents) . Were the relevant data available, these complex interactions could be analyzed using multilevel methods
. Even absent these more detailed data, however, using only ABSMs we could still detect marked—yet typically undocumented–socioeconomic gradients in health within diverse racial/ethnic-gender groups plus provide conservative estimates of their contribution to racial/ethnic health disparities.
Even so, caution is required regarding interpretation of our data in relation to race/ethnicity. This is because our estimates of the magnitude of socioeconomic inequalities in health, within and across diverse racial/ethnic groups, necessarily are subject to concerns about racial/ethnic misclassification and the census undercount . By itself, the method of geocoding and employing area-based socioeconomic measures cannot directly address these two problems, which affect all population-based analyses reliant on public health surveillance and census data
. Recent analyses, however, suggest that these problems result in estimates of US death rates among the white and black population being overstated in official publications by only 1% and 5%, respectively, and being understated, by a similar degree, for Hispanics (by 2%), but by a much larger degree for American Indians (by 21%) and Asian or Pacific Islanders (by 11%)
. Similar patterns have been reported for cancer registry data
and likely would affect the other outcomes (i.e., STI, TB, and injuries) also reliant on census denominators and total or partial use of non-self-report data on race/ethnicity. Such errors would result in a tendency to overestimate, compared to the white population, an excess risk among the black population and a reduced risk among the Hispanic population. Analyses of low birth weight and childhood lead poisoning, by contrast, would not be affected by the census undercount, since the denominators were, respectively, the births themselves and the children screened; moreover, racial/ethnic misclassification was minimized by use of self-report racial/ethnic data in these surveillance systems.
An additional caveat pertains to our use of the US poverty line as an indicator of socioeconomic deprivation. Although debates exist over how best to measure poverty in the US , precisely because of its significance for policies and for resource allocation
, evidence indicates the CT poverty measure, especially in excess of 20% (the federal definition of a “poverty area”
, does provide a reasonable decennial indicator of neighborhood economic deprivation, as assessed in relation to housing deterioration, refuse, crime, and other social indicators (e.g., unemployment, low earnings, low education)
. Also underscoring the robustness of the CT poverty measure as a useful economic indicator, we found similar results
in analyses utilizing data on the percent of persons below 50% of the US poverty line, above 200% of the US poverty line, and below 50% of the US median household income (an alternative measure of poverty employed in many European countries
. In all of these analyses, the magnitude of the socioeconomic gradients detected were on par with available estimates reported in the US
and analogous European literature
., The net implication is use of the CT poverty measure is unlikely to overestimate either the extent of socioeconomic gradients or their contribution to racial/ethnic disparities in health, and instead provides a useful metric that reveals the widespread and often profound extent to which socioeconomic deprivation adversely shapes population health, from infancy to death.
In conclusion, results of our study highlight the importance—and feasibility–of routinely monitoring US socioeconomic inequalities in health, overall and stratified by race/ethnicity and gender, thereby painting a truer picture of the “public-health situation as a whole,” as long urged by Sydenstricker and other public health leaders . Addressing gaps in policy-relevant knowledge
, the evidence generated by our approach could be used to set health objectives, guide resource allocation, and track progress—and setbacks–in reducing social disparities in both health and health care, at the national, state, and local level. Relying on widely-available data, the proposed methodology not only is cost-efficient but also permits comparisons within and across health outcomes throughout the US, over time, based on a common metric for socioeconomic position derived from US census data. Timeliness of CT data, moreover, will be improved, starting in 2008, when the American Community Survey starts releasing annual CT estimates, based on 5-year rolling averages
. Were data on US socioeconomic inequalities in health readily available, and reported upon yearly, for both the total population and diverse racial/ethnic-gender groups, efforts to track—and improve accountability for addressing—social disparities in health would be greatly enhanced. We suggest this can be accomplished by geocoding US public health surveillance data and using the CT-level measure “percent of persons below poverty.”
In the rest of this monograph, we explain our methods to facilitate their use by others. Specific sections focus on:
- how we geocoded our data;
- how we constructed the ABSMs;
- how we tested these measures across diverse health outcomes at different geographic levels;
- how we generated our figures; and
- a guided exercise, using a sample data file, to facilitate trying out our approach, with steps clearly delineated and answers provided to check accuracy of implementation.
We hope you will find this monograph useful in improving efforts to monitor socioeconomic inequalities in health, both within the total population and diverse racial/ethnic-gender groups, thereby making a vital contribution to identifying and galvanizing action to address social disparities in health.
REFERENCES
1. National Center for Health Statistics. Health, United States, 1998 with Socioeconomic Status and Health Chartbook. Hyattsville, MD: US Dept of Health and Human Services, 1998.
2. Evans T, Whitehead M, Diderichsen F, Bhuiya A, Wirth M (eds). Challenging inequities in health: from ethics to action. Oxford, UK: Oxford University Press, 2001.
3. Shaw M, Dorling D, Gordon D, Davey Smith G. The Widening Gap: Health Inequalities and Policy In Britain. Bristol, UK: The Policy Press, 1999.
4. Krieger N, Rowley DL, Herman AA, Avery B, Phillips MT. Racism, sexism, and social class: implications for studies of health, disease, and well-being. Am J Prev Med 1993; 9 (Suppl):82-122.
6. Krieger N, Chen JT, Ebel G. Can we monitor socioeconomic inequalities in health? A survey of U.S. Health Departments’ data collection and reporting practices. Public Health Rep 1997; 112:481-91.
8. Krieger N. The making of public health data: paradigms, politics, and policy. J Public Health Policy 1992; 13:412-427.
9. Williams DR, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Annu Rev Sociol 1995; 21:349-86.
10. Kington RS, Nickens HW. Racial and ethnic differences in health: recent trends, current patterns, future directions. In: National Research Council. America becoming: racial trends and their consequences. Vol 2. Smelser NJ, Wilson WJ, Mitchell F (eds). Washington, DC: National Academy Press, 2001; 253-310.
11. Navarro V. Race or class versus race and class. Lancet 1990; 336:1238-40.
12. Pantazis C, Gordon D (eds). Tackling Inequalities: Where Are We Now and What Can Be Done? Bristol, UK: The Policy Press, 2000.
13. Marmot M, Wilkinson RG (eds). Social Determinants of Health. Oxford: Oxford University Press, 1999.
14. Porter D (ed). The History of Public Health and the Modern State. Amsterdam; Atlanta, GA: Rodopi, 1994.
15. National Center for Health Statistics. Health, United States 2002 with Chartbook on Trends in the Health of Americans. Hyattsville, MD: National Center for Health Statistics, 2002.
16. Braveman P, Starfield B, Geiger HJ. World Health Report 2000: how it removes equity from the agenda for public health monitoring and policy. Br Med J 2001;323:678-81.
17. Sydenstricker E. The incidence of illness in a general population group: General results of a morbidity study from December 1, 1921 through March 31, 1924, Hagerstown, Md. Public Health Rep 1925;40:279-91.
18. Sydenstricker E. Health and the Depression. Milbank Memorial Fund Quarterly 1934: 12:273-280.
19. US Department of Health, Education, and Welfare. Origin and Program of the U.S. National Health Survey. Health Statistics Series A1, May 1958, p. 3.
20. Winslow C-EA. The Life of Hermann M. Biggs, M.D., D.Sc., LL.D, Physician and Statesman of the Public Health. Philadelphia, PA: Lea & Febiger, 1929.
21. Rosen G. A History of Public Health. (1958). Introduction by Elizabeth Fee; Bibliographical essay and new bibliography by Edward T. Morman. Expanded ed. Baltimore, MD: Johns Hopkins University Press, 1993.
22. Krieger N, Williams D, Moss N. Measuring social class in US public health research: concepts, methodologies and guidelines. Annu Rev Public Health 1997; 18:341-378.
23. Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health 1992; 82:703-710.
24. Lynch J, Kaplan G. Socioeconomic position. In: Berkman L, Kawachi I (eds). Social Epidemiology. Oxford: Oxford University Press, 2000; 13-35.
25. Lee P, Murie A, Gordon D. Area Measures of Deprivation: A Study of Current Methods and Best Practices in the Identification of Poor Areas in Great Britain. Birmingham, UK: Centre for Urban and Regional Studies, University of Birmingham, 1995.
26. Carstairs V. Socio-economic factors at areal level and their relationship with health. In: Elliott P, Wakefield J, Best N, Briggs D (eds). Spatial Epidemiology: Methods and Applications. Oxford: Oxford University Press, 2000; 51-67.
27. Nathan WB. Health Conditions In North Harlem 1923-1927. New York: National Tuberculosis Association; 1932.
28. Green HW. The use of census tracts in analyzing the population of a metropolitan community. J Am Stat Assoc 1933; 28:147-153.
29. Terris M. Relation of economic status to tuberculosis mortality by age and sex. Am J Public Health 1948; 38:1061-70.
30. Coulter EJ, Guralnick L. Analysis of vital statistics by census tract. J Am Stat Assoc 1959; 54:730-40.
back to top
32. Krieger N. Epidemiology and the web of causation: has anyone seen the spider? Soc Sci Med 1994; 39:887-903.
33. Krieger N. Theories for social epidemiology for the 21st century: an ecosocial perspective. Int J Epidemiol 2001; 30:668-677.
38. Rossi RJ, Gilmartin KJ. The Handbook of Social Indicators: Sources, Characteristics, and Analysis. New York, NY: Garland STPM Press, 1980.
42. US Bureau of Census. Census of population and housing, 1990: Summary Tape File 3 technical documentation. Washington, DC: Bureau of the Census, 1991.
43. US Bureau of the Census. Poverty areas.
44. Singh GK, Miller BA, Hankey BF, Edwards BK. Area Socioeconomic Variations in U.S. Cancer Incidence, Mortality, Stage, Treatment, and Survival, 1975-1999. NCI Cancer Surveillance Monograph Series, Number 4. Bethesda, MD: National Cancer Institute, 2003. (NIH Pub. No. 03-5417).
45. Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Soc Sci Med 2002;55:125-39.
46. O’Campo P. Invited commentary: advancing theory and methods for multilevel models of residential neighborhoods and health. Am J Epidemiol 2003;157:9-13.
47. Subramanian SV, Jones K, Duncan C. Multilevel methods for public health research. In: Kawachi I, Berkman L (eds). Neighborhoods and Health. Oxford: Oxford University Press 2003:65-111.
48. Rosenberg HM, Maurer JD, Sorlie PD, Johnson NJ, MacDorman MF, Hoyert DL, Spitler JF, Scott C. Quality of death rates by race and Hispanic origin: a summary of current research, 1999. National Center for Health Statistics, Vital Health Stat 2(128), 1999.
49. Keppel KG, Pearcy JN, Wagener DK. Trends in racial and ethnic-specific rates for health status indicators: United States, 1990-1998. Healthy People 2000 Statistical Notes, no. 23. Hyattsville, MD: National Center for Health Statistics, January 2002.
50. United States Cancer Statistics Working Group. United States Cancer Statistics: 1999 Incidence. Department of Health and Human Services, Atlanta, GA: Centers for Disease Control and Prevention and National Cancer Institute 2002.
51. Citro CF, Michael RT (eds). Measuring Poverty: A New Approach. Panel on Poverty and Family Assistance: Concepts, Information Needs, and Measurement Methods. Washington, DC: National Academy Press, 1995.
52. Citro CF, Kalton G (eds). Small-Area Income and Poverty Estimates: Priorities for 2000 and Beyond. Panel on Estimates of Poverty for Small Geographic Areas, Committee on National Statistics, Commission on Behavioral and Social Sciences and Education, National Research Council. Washington, DC: National Academy Press, 2000.
53. Gordon D, Spicker P (ed). The International Glossary on Poverty. London: Zed Books, 1999.
54. Jargowsky PA. Poverty and Place: Ghettos, Barrios, and The American City. New York: Russell Sage, 1997.
55. Krieger N, Fee E. Measuring social inequalities in health in the United States: an historical review, 1900-1950. Int J Health Serv 1996;26:391-418.
56. Fiscella K, Franks P, Gold M, Clancy C. Inequalities in quality: addressing socioeconomic, racial and ethnic disparities in health care. JAMA 2000; 283:2579-84.
57. Friedman D, Anderka M, Krieger J, Land G, Solet D. Accessing population health information through interactive systems: lessons learned and future directions. Public Health Rep 2001; 116:132-41.
58. US Census Bureau. Survey Basics: What is the American Community Survey? (Accessed on February 5, 2004 at: http://www.census.gov/acs/www/SBasics/What/What1.htm ).




You must be logged in to post a comment.