[ Spring 2008 ]
The world is finally waking up to male circumcision
The Harvard School of Public Health’s Daniel Halperin has been something of a maverick in the field of HIV/AIDS research. A medical anthropologist and an epidemiologist—one who scours populations for clues to what might cause disease—Halperin was among the first to spotlight signs that male circumcision could be a pivotal link in the AIDS pandemic.
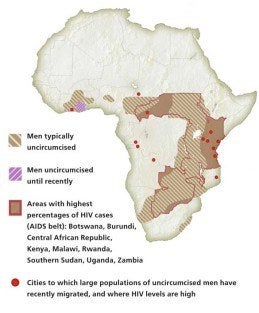
More than 20 years ago, the earliest observers noted that African regions with the lowest HIV infection rates were also those where circumcision was most widely practiced. By 1999, Halperin and Robert Bailey of the University of Illinois in Chicago argued in a review and data analysis for the Lancet that the evidence was “compelling.” Yet only last year did the World Health Organization (WHO) finally put its stamp of approval on circumcising men as one way—along with behavioral changes and other strategies—to help prevent transmission of the AIDS virus, especially in Africa.
Before joining HSPH’s Harvard Center for Population and Development Studies in 2006, Halperin, now a senior research scientist and lecturer in international health, worked as an advisor to USAID’s Southern African Regional HIV/AIDS Program, based in Swaziland, where 26 percent of adults are HIV-positive.
Halperin answers questions on this research, below.
What does male circumcision have to do with the spread of HIV/AIDS?
Clinicians have suspected for decades that the foreskin is a portal of entry for HIV. The main reason is that its inner surface is not highly keratinized.
[Keratin is a protective layer, a protein that covers most skin.] This mucous membrane is permeable, prone to tearing and lesions, and dense with cells targeted by HIV. During sex, the foreskin is pulled back, and most heterosexual HIV transmission happens through the foreskin’s inner surface.
There’s an urban legend that women are biologically more vulnerable to HIV. It is true if men are circumcised, but not if they aren’t. Men, if anything, may be somewhat more vulnerable than women because of that foreskin. It’s an Achilles’ heel, biologically, for men.
How were you and some others seeing this play out in Africa?
Even before I was seriously studying HIV/AIDS, the anthropologist Priscilla Reining—in the mid to late eighties, in Tanzania—noticed some groups were decimated by AIDS while others nearby weren’t nearly as affected. But there was no discernible difference in sexual practices; the difference was whether groups were practicing male circumcision or not. And Canadian researchers looked at men visiting prostitutes in Nairobi over several years and included circumcision as a factor. Lo and behold, eight to ten times as many men who were uncircumcised got infected.
What role have you played in looking at this issue?
Ten or 15 years ago, there was just a tiny number of us working on this. It was considered an exotic or strange thing even to be talking about. We’d even get ridiculed at conferences and so on. Now, it’s accepted.
I got interested in it because the epidemiology was so stunning. I started noticing a number of studies of risk factors for HIV in Africa and almost inevitably, male circumcision would stand out as the number one or two variable in the analysis. That led to the drafting of our 1999 Lancet article, which pulled together various epidemiological and biological studies.
Until then, there was relatively little attention or discussion of male circumcision. Some later studies really jolted the scientific community. They could no longer ignore this issue.
So, if we’ve known for the last nine years or more that there’s such a convincing correlation between male circumcision and rates of HIV infection, what took scientists and the public health community, both governmental and non-governmental, so long to take decisive action?
The argument was that it was a surgical procedure, and that until we had the highest level of evidence—from multiple randomized, controlled trials—all this observational data could be due to other complicating factors. In one part of Uganda, for example, almost all the men circumcised were Muslims, and some scientists there felt maybe it was being a Muslim that protected them from HIV because of certain sexual or hygienic practices.
There’s also been a bias toward high-tech solutions. Most AIDS programs have been run by medical doctors, who are very smart, good people, yet who by training tend to look for the technological bullet—medicine, vaccines, condoms. The assumption was that circumcision was a “cultural” issue, and there’s always been this fear of treading in that territory.
What most people didn’t realize is that, if the data had found circumcision actually increased the risk of HIV and you were trying to dissuade those cultures from circumcising men, it would be an extremely difficult undertaking. People assumed the converse was true: that other cultures felt it was important to not circumcise. That turns out, for the most part, to be untrue. In most places in Africa where men are not circumcised, it’s not particularly important for that culture. According to one Harvard study, over 80 per cent of men in Botswana said they’d like to be circumcised, even without knowing of the HIV-prevention benefit.
You’ve written that male circumcision would work like a vaccine against HIV, and could be very cost-effective. What are your hopes that this solution will really take off?
There’s a lot more interest in it now. The U.S. foreign AIDS program has said they will fund circumcision services if they receive a written request from the government. Rwanda, Kenya, Swaziland, and some others are asking for this. It’s a little slow, but it’s coming along. There’s been a significant increase in funding for male circumcision by the U.S. government. Apparently, it’s gone up almost 30-fold, from $600,000 last year to $16 million this year. But if you think about it, $16 million out of about $6 billion a year in U.S. foreign assistance for HIV/AIDS is still a drop in the bucket.
But if there’s a widespread uptake in male circumcision in parts of Africa with high HIV prevalence, the long-term benefits could be huge. WHO and UNAIDS estimate that some three million deaths could be averted over the next 20 years, many of them women’s.
To hear Halperin’s podcast comparing circumcision with other HIV/AIDS prevention strategies, go to www.hsph.harvard.edu/multimedia/audio/2008/halperin/. For links to his recent policy paper fromScience and other articles, visit www.harvardaidsprp.org/daniel-halperin.html.
Freelance journalist Christopher Burrell has written for the New York Times, Washington Post, and Boston Globe Magazine, and produced shows for WBUR-Boston and National Public Radio.