Overview
Nick Menzies is Associate Professor of Global Health in the Department of Global Health and Population, and part of the core faculty of the Harvard Center for Health Decision Science. Professor Menzies uses decision science and quantitative research to understand the consequences of policies to combat major infectious diseases, and help design effective disease control programs when resources are limited.
Research
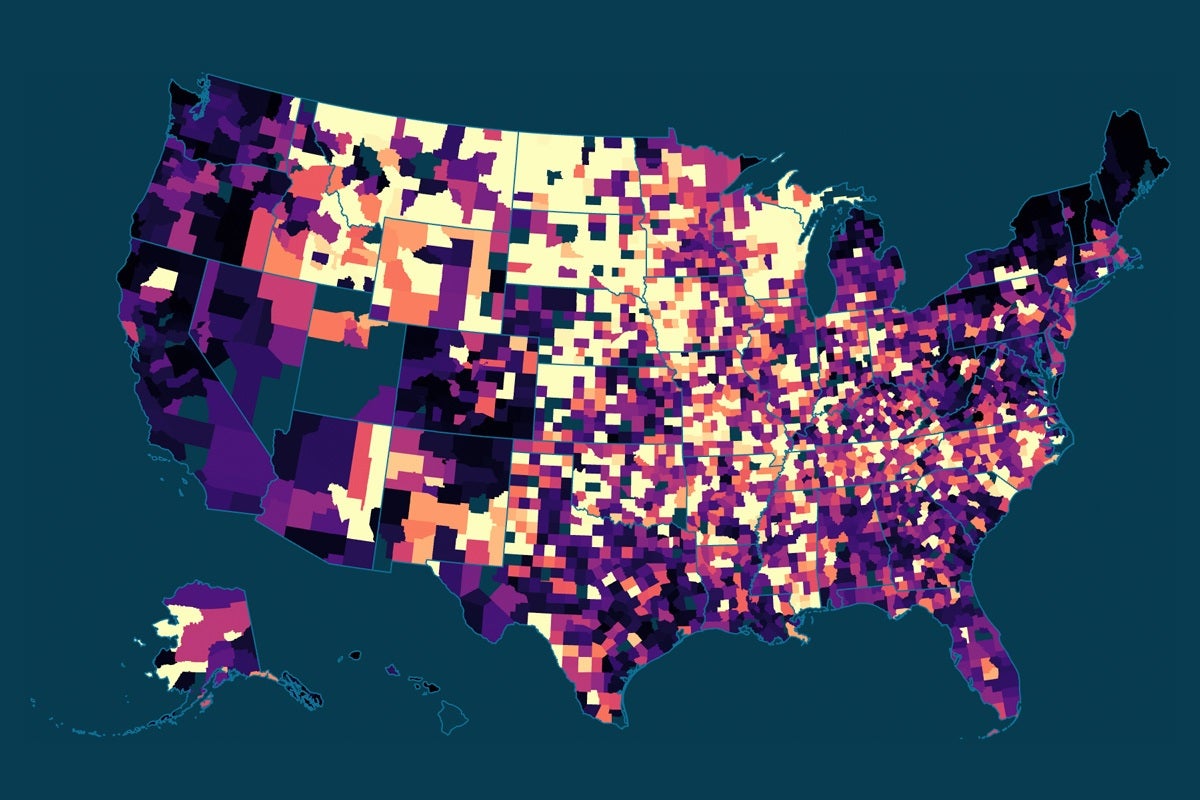
Professor Menzies combines empirical data with mathematical modeling to examine infectious disease control policy in high burden settings, currently focusing on the intersection of HIV and TB epidemics in sub-saharan Africa and other high-burden settings.
In his empirical research Nick has worked to improved the level of evidence on the resource requirements for HIV interventions in high burden settings, allowing for better budgeting of these large programs and allowing decision-makers to weigh the advantages of different implementation approaches. Nick is currently working on a multi-country study to understand the costs, cost drivers and efficiency determinants of routine immunization services. Other applied work has addressed the costs and benefits of expanding access to HIV screening and diagnosis in high prevalence settings.
The long-term population-level impacts of disease control policy are often difficult to assess empirically, especially for infectious diseases. Yet these are often the outcomes of interest when planning major public health investments. Through a number of studies Nick has used mathematical modelling - computer experiments which seek to recreate the underlying mechanisms generating health outcomes and resource utilization - to compare competing policy options being considered by HIV or TB control programs and directly inform the policy debate.
Professor Menzies's methodological interests include Bayesian approaches to calibrating simulation models, value of information analysis, the use of simulation models for causal inference, and approaches for synthesizing results from multiple models to inform policy.
Prior to joining Harvard Nick worked with the Global AIDS Program at the U.S. Centers for Disease Control and Prevention, conducting economic evaluation and implementation research on HIV/AIDS control interventions in countries supported by the President's Emergency Plan for AIDS Relief (PEPFAR).