For Immediate Release: March 12, 2008
Boston, MA — A novel aerosol version of the most common tuberculosis (TB) vaccine, administered directly to the lungs as an oral mist, offers significantly better protection against the disease in experimental animals than a comparable dose of the traditional injected vaccine, researchers report this week in the Proceedings of the National Academy of Sciences.
The aerosol vaccine — under development through a collaboration between Harvard University and the international not-for-profit Medicine in Need (MEND) — could provide a low-cost, needle-free TB treatment that is highly stable at room temperature.
“Rising rates of tuberculosis and drug-resistant disease in developing countries have amply illustrated the need for more effective vaccines,” says David Edwards, the Gordon McKay Professor of the Practice of Biomedical Engineering in Harvard’s School of Engineering and Applied Sciences. “While most new TB vaccines continue to call for needle injection, our vaccine could provide safer, more consistent protection by eliminating these injections and the need for refrigerated storage. We see great promise for this new treatment.”
Says Barry R. Bloom, Dean of the Harvard School of Public Health: “Tuberculosis is one of the most resistant and challenging diseases to protect against, and the successful results of aerosol delivery using nanoparticle technology offers a potentially new platform for immunization. Were the animal results here confirmed in human studies, this technology could be used not only for TB vaccines, but those protecting against other infectious diseases as well.”
The current PNAS paper by Edwards, Bloom, and colleagues at the University of North Carolina-Chapel Hill, the Aeras Global TB Vaccine Foundation, MEND South Africa, the Harvard School of Public Health and School of Engineering and Applied Sciences, and Manta is based on studies involving guinea pigs, a species of rodent highly sensitive to TB.
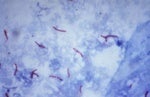
Among guinea pigs vaccinated with the aerosol treatment and subsequently exposed to TB, less than 1 percent of lung and spleen tissue showed effects of the disease. By contrast, in animals treated with the same dose of the traditional injected vaccine, some 5 percent of lung tissue and 10 percent of spleen tissue showed symptoms following TB exposure.
Administered to 100 million infants annually, the current Bacillus Calmette-Guérin (BCG) vaccine for TB is the world’s most widely administered childhood vaccine. Dried into a powder by freezing and delivered by needle injection, the vaccine requires refrigerated storage and has shown variable degrees of protection against tuberculosis in different parts of the world. These limitations have prompted calls from public health experts and physicians for alternative treatments.
The rapid-drying process by which the aerosol vaccine is made resembles the technique used in the manufacture of powdered milk. In the aerosol vaccine, particles form at micrometer and nanometer scales and in spherical and elongated shapes, a combination that appears to improve dispersal in the mouth.
While commonly used with food, cosmetics, and pharmaceuticals, this spray drying of small and large molecules is seldom used for drying cellular material. The new technique enables TB vaccines, and potentially other bacterial and viral-based vaccines, to sidestep the traditional problems associated with keeping vaccines chilled.
“Spray drying is lower-cost than BCG, easily scalable for manufacturing, and ideal for needle-free use, such as via inhalation,” says Edwards, an international leader in aerosol drug and vaccine delivery. “Its greater stability at room temperature could ultimately provide a better means of creating and delivering vaccine throughout the world.”
Edwards and Bloom’s co-authors are Anthony Hickey, Lucila Garcia-Contreras, Pavan Muttil, and Danielle Padilla, all of UNC-Chapel Hill; Yun-Ling Wong, Jessica DeRousse, and Katharina Elbert of Harvard’s School of Engineering and Applied Sciences; Jerry Sadoff of the Aeras Global TB Vaccine Foundation; Willem Andreas Germishuizen and Bernard Fourie of MEND South Africa; Sunali Goonesekera of the Harvard School of Public Health; and Rich Miller of Manta. The research was supported by a Grand Challenge Grant from the Bill and Melinda Gates Foundation.
Contact:
Christina Roache
617-432-6052
croache@hsph.harvard.edu
Steve Bradt
617-496-8070
steve_bradt@harvard.edu
###
Harvard School of Public Health is dedicated to advancing the public’s health through learning, discovery, and communication. More than 400 faculty members are engaged in teaching and training the 1,000-plus student body in a broad spectrum of disciplines crucial to the health and well being of individuals and populations around the world. Programs and projects range from the molecular biology of AIDS vaccines to the epidemiology of cancer; from risk analysis to violence prevention; from maternal and children’s health to quality of care measurement; from health care management to international health and human rights. For more information on the school visit: https://www.hsph.harvard.edu