Experimental findings could lead to new, inexpensive therapy using a naturally occurring bile acid
For immediate release: Wednesday, November 13, 2013
Boston, MA – New research led by Harvard School of Public Health (HSPH) demonstrates a disease mechanism in type 1 diabetes (T1D) that can be targeted using simple, naturally occurring molecules to help prevent the disease. The work highlights a previously unrecognized molecular pathway that contributes to the malfunction of insulin-producing pancreatic beta cells in T1D in human patients and in mice, and shows that a chemical intervention can help beta cells function properly and survive. Currently, there is no preventive regimen or cure for T1D, and the only treatment is insulin therapy by injection or pump.
The study appears online November 13, 2013 in Science Translational Medicine.
In T1D, beta cells are mistakenly attacked by the body’s own immune system, and much prior research has focused on ways to prevent this autoimmune response. “This study breaks new ground because it focuses on boosting beta cell performance and shows that beta cell preservation is possible even in the face of such immune attack,” said senior author Gökhan S. Hotamisligil, chair of the Department of Molecular Metabolism and J.S. Simmons Professor of Genetics and Metabolism at HSPH.
It’s estimated that as many as three million Americans have T1D. According to the National Institute of Diabetes and Digestive and Kidney Diseases, each year more than 15,000 children and 15,000 adults—roughly 80 people per day—are diagnosed with the disease in the U.S. And the numbers are on the rise: according to the U.S. Centers for Disease Control and Prevention, the disease’s prevalence in Americans under age 20 rose by 23% between 2001 and 2009.
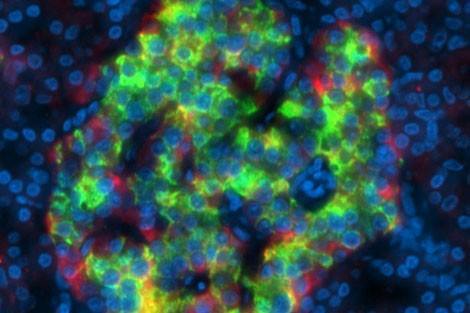
Using human pancreatic samples and mouse models, the HSPH researchers—with colleagues from Harvard Medical School, the Broad Institute of Harvard and MIT, and the Université Libre de Bruxelles—sought to tease apart the mechanisms of beta cell failure in T1D. They homed in on the function of the endoplasmic reticulum (ER)—a “mini-organ” inside cells where proteins and lipids are processed and packaged and undergo quality control before they reach their destinations in the body. The ER is known to play a critical role in supporting the work of beta cells.
The researchers found that, in animal models and in humans with T1D, ER function is compromised by the immune attack. This reduced ER function results in ER stress and contributes to the death of beta cells and the insulin insufficiency that is characteristic of T1D.
In earlier studies, researchers in the Hotamisligil lab showed that ER stress in other tissues plays a key role in obesity and type 2 diabetes, and can be corrected with so-called “chemical chaperones” such as tauroursodeoxycholic acid (TUDCA), a bile acid. Based on that previous research, the scientists applied TUDCA to mouse models of T1D. They found that ER function improved—both in mice with diabetes and those with pre-diabetes. Beta cells functioned better and were less likely to die, and, to the researchers’ surprise, the treated mice had a dramatically reduced incidence of T1D. The researchers also identified the specific molecular pathway through which TUDCA influences ER function.
“The study is exciting because it suggests that improving ER function before the onset of disease could reduce T1D incidence,” said lead author Feyza Engin, research associate in the HSPH Department of Molecular Metabolism.
Advances in medicine now allow physicians to identify, with great accuracy, those with very high risk for developing T1D. “There is really a need for some safe and mild interventions that can prevent emergence of type 1 diabetes in these populations,” said Hotamisligil. “TUDCA is safe and inexpensive. It’s possible that TUDCA or another molecule that acts via the described mechanisms could be used as a novel therapeutic approach to keep those at risk for type 1 diabetes disease-free for long periods of time, or could even prevent the disease all together.”
Other HSPH authors included Alena Yermalovich, Truc Nguyen, and Sarah Hummasti, all members of the Hotamisligil lab.
Funding for this project was provided by JDRF (17-2008-901); National Institutes of Health PO1 (A1054904); the European Union; the Fonds National de la Recherche Scientifique; and Schuylar funds.
“Restoration of the Unfolded Protein Response in Pancreatic β Cells Protects Mice Against Type 1 Diabetes,” Feyza Engin, Alena Yermalovich, Truc Nguyen, Sarah Hummasti, Wenxian Fu, Decio L. Eizirik, Diane Mathis, and Gökhan S. Hotamisligil, Science Translational Medicine, Vol. 5, Issue 211, online November 13, 2013
For more information:
Marge Dwyer
617.432.8416
mhdwyer@hsph.harvard.edu
Image: Feyza Engin
###
Harvard School of Public Health brings together dedicated experts from many disciplines to educate new generations of global health leaders and produce powerful ideas that improve the lives and health of people everywhere. As a community of leading scientists, educators, and students, we work together to take innovative ideas from the laboratory and the classroom to people’s lives—not only making scientific breakthroughs, but also working to change individual behaviors, public policies, and health care practices. Each year, more than 400 faculty members at HSPH teach 1,000-plus full-time students from around the world and train thousands more through online and executive education courses. Founded in 1913 as the Harvard-MIT School of Health Officers, the School is recognized as the oldest professional training program in public health.