Miguel Martínez-González discussed contradictory findings on alcohol and health during the Department of Nutrition’s 18th annual Stare-Hegsted lecture.
October 12, 2023 — There’s a large body of research pointing to a link between alcohol consumption and reduced risk of cardiovascular disease. But studies in recent years have contradicted these findings, suggesting that no amount of alcohol is safe for health. Physician and researcher Miguel Martínez-González recently outlined the controversy for a Harvard T.H. Chan School of Public Health audience, exploring whether alcohol—particularly red wine—still has a place in healthy eating plans such as the Mediterranean diet.
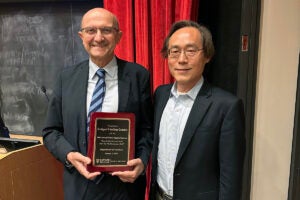
Martínez-González is the principal investigator on PREDIMED-PLUS, a Mediterranean diet and lifestyle clinical trial focused on prevention of cardiovascular disease. He is an adjunct professor of nutrition at Harvard Chan School and a professor of preventive medicine and public health at the University of Navarra in Spain. He delivered the 18th annual Stare-Hegsted Lecture on October 2 in Kresge G-2 to a hybrid audience. The event, sponsored by the Department of Nutrition, honors department founders Fredrick Stare and D. Mark Hegsted.
Research by Martínez-González and colleagues has found that a Mediterranean diet including alcohol reduced risk of cardiovascular disease by 30% compared to a low-fat diet which did not specifically include alcohol.
In another study, they found that people who followed what the researchers defined as a moderate Mediterranean drinking plan—choosing red wine, drinking with meals, and spreading consumption over the course of the week—had a lower risk of mortality than people who abstained from alcohol. Martínez-González noted that additional recent studies have found that light to moderate alcohol consumption lowered the relative risks for premature mortality, and mortality from cancer and cardiovascular disease.
However, Martínez-González noted that alcohol’s potential harms must be considered, particularly for young people. One out of every four deaths of Americans ages 20 to 34 can be attributed to alcohol, he said, noting that in addition to increasing the risk of accidental deaths, alcohol may also increase the risk of breast cancer. Some imaging studies of the brain suggest that alcohol may be toxic to neurons, Martínez-González said, adding that it is more broadly toxic to the body if consumed in large amounts.
“So, should we remove wine from the Mediterranean diet?” he asked. “Yes, definitely for those under 35 years.” But for older adults, it’s more complicated. He and his colleagues, and other researchers, have found that the Mediterranean diet loses up to 23.5% of its protective effect if wine is removed.
Randomized controlled trials are needed to ensure that potential benefits or harms from alcohol consumption are adequately assessed, Martínez-González said. He and his colleagues at the University of Navarra received funding for such a study earlier this year. The study is recruiting physicians ages 50 to 75, who will be randomized to moderate drinking or abstention groups. Both groups will receive free beverages—red wine or an alcohol-free alternative—during the five-year study.
Martínez-González hopes that this trial will help clarify whether red wine should be part of the Mediterranean diet for adults over 35.
Photos: iStock / webphotographeer, Brett Otis
