December 8, 2017 – A research team at Harvard T.H. Chan School of Public Health has identified a key metabolic vulnerability in some types of tumor cells and discovered a way to exploit it by harnessing well-known immunosuppressant drugs. Their studies, carried out in cells and mice and published last month in Cancer Cell, reveal that the drugs can selectively kill tumor cells while sparing normal cells. The research suggests that these immunosuppressants, which have been in clinical use for several decades for autoimmune disorders and transplant surgery, could be repurposed as effective treatments for some forms of cancer.
“The genetic makeup of a tumor cell can reprogram its metabolism in a way that creates a vulnerability that we can target with a drug,” said Brendan Manning, professor of genetics and complex diseases at Harvard Chan School and senior author of the study. “Here, we’ve uncovered an important — and readily exploitable — vulnerability in cells that have chronic activation of a critical pro-growth pathway, known as the mTOR pathway.”
Scientists have known for decades that cancer cells’ metabolism differs from normal cells’ metabolism. Tumors tend to grow at an impressive clip, increasing both in number and size. So the cells require plenty of nutrients as well as the molecular building blocks that support their growth.
Manning and his colleagues have spent several years dissecting the molecular signals and corresponding nutrient demands that underpin tumor cell growth, including those triggered by a special protein called mTOR (also known as mTORC1, for Mechanistic Target Of Rapamycin Complex 1). Normally, mTOR activity is under very tight control, switched on only when sufficient nutrients and specific growth factors are present. But in the majority of cancer cells, it is stuck in an always-on state.
Importantly, drugs such as rapamycin, sirolimus, and others can inhibit the activity of mTOR. They have undergone clinical testing for potential treatment of a variety of cancers, but when administered as single agents, the outcomes have been disappointing. “These drugs can slow tumor growth, but they don’t kill the tumor,” said Manning. “So that was part of our motivation to search for metabolic vulnerabilities that arise when mTOR is in a ‘locked-on’ state and could make tumor cells more susceptible to attack.”
In earlier studies, Manning’s team revealed that a key role of mTOR is to instruct cells to make nucleotides — the genetic building blocks that get strung together to make nucleic acids, such as DNA (which spells out the cells’ genetic blueprint) and RNA (used to make proteins). Could this demand to make nucleotides represent a molecular Achilles’ heel that could be targeted to destroy tumor cells with uncontrolled mTOR signaling?
“This was an attractive process for us to target because there are a number of clinically approved and safe inhibitors of nucleotide synthesis pathways, which are used throughout the world, most commonly as immunosuppressants,” said the study’s first author, Alexander Valvezan, postdoctoral research fellow at Harvard Chan School.
To test this idea, Valvezan and colleagues turned to cell and animal models of a human tumor syndrome, called tuberous sclerosis complex (TSC). Patients with TSC develop spontaneous, benign tumors in the brain and other critical organs, including the heart, lungs, kidney, liver, and skin. At a molecular level, the disorder is characterized by hyperactivity of mTOR, thereby offering an ideal test bed for finding the sort of molecular weakness the research team was seeking.
They discovered that a nucleotide synthesis inhibitor known as mizoribine had a dramatic effect: It killed the tumor cells, while sparing normal cells in a Petri dish. Moreover, it also showed tumor-killing capabilities in mouse models of TSC, shrinking and eliminating existing tumors in animals with advanced disease, and completely preventing tumor growth in animals with early-stage disease.
“Because these inhibitors have been used clinically for decades, we know that they’re safe,” said Valvezan. “This makes them very attractive candidates for subsequent clinical testing to evaluate their therapeutic effects in TSC and possibly cancers with overactive mTOR.”
As the scientists’ searched for a molecular explanation for mizoribine’s anti-tumor effects, they highlighted an important, but often overlooked, aspect of cells’ metabolism. When cells receive growth signals, like those from mTOR, they ramp up production of the components needed to support their growth. Those include DNA as well as RNA, which are both made from nucleotides. That means DNA production and RNA production are effectively competing for the cells’ nucleotides. “There’s an underappreciated tug of war on the nucleotide pool,” said Manning.
“When mTOR is in overdrive, it preferentially directs nucleotides toward RNA, so when you come in with a drug that decreases nucleotide production it hits the pool available for DNA the hardest, causing severe stress on the cancer cell and ultimately, cell death.” Normal cells with low mTOR activity are spared because the rate of RNA production is much lower, leaving sufficient nucleotides to support DNA synthesis.
While Manning and his colleagues are excited by their findings, they caution that this research is only a first step. Before mizoribine or related drugs can be considered as a potential anti-tumor treatment, the scientists must extend these initial results to other tumor settings, and potentially through future clinical trials.
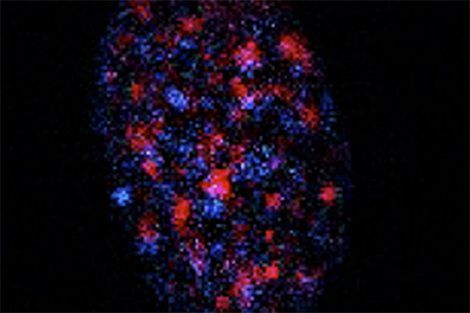
photo: Manning Lab