The most powerful influences on population health are not the medical interventions that diagnose and treat disease. Rather, they are the broad social forces—war or peace, poverty or financial security, political oppression or fundamental human rights—that shape all of our life possibilities. In the U.S. and across the globe, Harvard School of Public Health has not only forged practical tools and strategies to alleviate suffering, but has also served as a moral voice in public health. The words inscribed in granite on the François-Xavier Bagnoud (FXB) Building—“the highest attainable standard of health is one of the fundamental rights of every human being”— come from the constitution of the World Health Organization, and form the bedrock of the School’s scholarship and fieldwork.
War and disaster
Tackling the nuclear threat
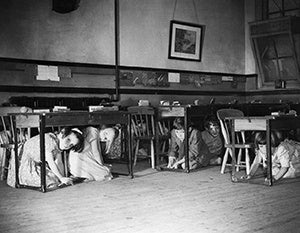
It was a time of fallout shelters, “duck and cover” exercises in elementary schools, and an ominous Cold War standoff between the United States and the Soviet Union. It was the late 1950s and, quite by chance, an eminent cardiologist and professor by the name of Bernard Lown attended a talk by Philip Noel-Baker, a recent British Nobel Peace laureate. He came away shaken. “Compared to the threatening nuclear disaster, sudden cardiac death, preoccupying me at the time, seemed a small problem,” Lown recalled, more than half a century later.
He decided to take action. In 1961, he mobilized a group of MDs—including Victor Sidel, Sidney Alexander, Jack Geiger, and Robert Goldwyn—into a group called Physicians for Social Responsibility, with the goal of convincing the public that nuclear war would decimate the population and poison the environment.
“How could we as physicians make a difference?” said Lown in a 2010 speech launching the Bernard Lown Scholars Program and Visiting Professorship at HSPH. “We extrapolated the medical consequences of a virtual nuclear bombing of Boston. We concluded that there was no meaningful medical response to a catastrophe of such magnitude. And we published our results in the New England Journal of Medicine.
“We became instant world experts on the topic,” added Lown, whose career highlights include developing the lifesaving direct current defibrillator. “Having demonstrated that in nuclear war there was no place to hide, our findings put an end to the underground shelter craze then exercising the American public.”
The son of Lithuanian Jews who had emigrated to the United States in 1935, Lown also saw disturbing parallels between the proliferation of nuclear weapons and Nazi Germany’s annihilation of 6 million Jews. “We destroyed Hitler and we became Hitlerized in our ability to design mass extermination,” he said in the 2010 speech.
In the 1970s, with the nuclear threat still looming, Lown reached out to an acquaintance—Evgeni Chazov, personal physician to Soviet leader Leonid Brezhnev and a collaborator on studies investigating sudden cardiac death. Lown asked Chazov if he’d consider joining forces with other U.S. colleagues—including Herb Abrams, Jim Muller, and Eric Chivian, founder of the Center for Health and the Global Environment at Harvard Medical School, as well as Drs. Mikhail Kuzin and Leonid Ilyin of the Soviet Union—to combat the nuclear threat. The result was International Physicians for the Prevention of Nuclear War (IPPNW), founded in 1980.
“Remarkably, within four years we gained 150,000 physician members in 60 countries and educated a wide public on the nuclear threat,” Lown said. “We did some seemingly impossible things.” The doctors sounded a medical warning to humanity: that nuclear war would be the final epidemic, and that there would be no cure and no meaningful medical response. Their message reached millions of people around the world. In the words of former New Zealand Prime Minister David Lange, “IPPNW made medical reality a part of political reality.”
In 1985, Lown and Chazov traveled together to Oslo to accept the Nobel Peace Prize on behalf of their organization.
World War II and today
Humanitarian assistance is in the DNA of Harvard School of Public Health. And one of the biggest public health and humanitarian relief efforts of the 20th century was the massive scale-up required to wage World War II.
HSPH graduate and future dean Brigadier General James Stevens Simmons served as head of the Preventive Medicine Service of the Army’s Office of the Surgeon General—the top public health official in the armed services. Simmons would boast of having trained 30,000 officers and enlisted men in various public health specialties by mid-1944.
When Oak Ridge, Tennessee, was chosen as the place to manufacture the fuel for the atomic bomb, it went from being a village of 19,000 to a bustling town of 78,000 almost overnight—and alum Bernard Blum, MPH ’38, was put in charge of keeping the inhabitants of the secret “atomic city” healthy.
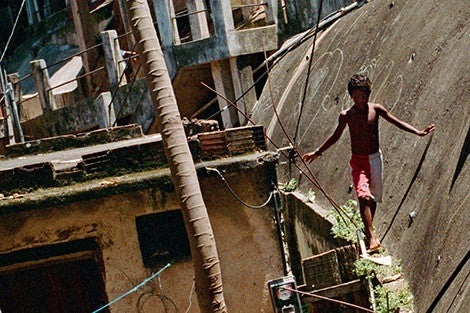
The war at homeUrban poverty and violence have long gone hand in hand, but to identify solutions, we need to understand how these problems intersect. Perhaps no one has contributed more to this effort than Professor of Human Behavior and Development Felton James Earls, whose research challenged the socalled broken windows theory that crime stems from community disrepair and disorder, arguing for its replacement with a theory of “collective efficacy”—the notion that neighborhood crime rates are tied to residents’ willingness to act for each other’s benefit, most particularly for the benefit of each other’s children. “It is far and away the most important research insight in the last decade,” Jeremy Travis, director of the National Institute of Justice from 1994 to 2000, told the The New York Times in 2004. Earls’ insights grew out of his massive Project on Human Development in Chicago Neighborhoods. Launched in 1994, the 10-year, $51 million epidemiological study, funded by the National Institute for Mental Health and the MacArthur Foundation, examined the causes and consequences of children’s exposure to violence. Not surprisingly, the recognition that urban violence is an urgent public health issue has deep roots at HSPH. Starting in the 1970s, physician Deborah Prothrow-Stith, as associate dean and professor of public health practice, advocated combating youth violence using strategies similar to those that had successfully curbed smoking and drunken driving. |
Granville Larimore, MPH ’42, served as chief of venereal disease education for the Army’s Office of the Surgeon General. Venereal disease was perhaps the most challenging infectious disease threat of the war, and in response, Larimore helped make a movie on venereal disease prevention, cleverly titled Pick Up.
Ruth Parmelee, MPH ’43, was assigned to an 8,000- person refugee camp in what was then called Palestine, where she encountered people infected with lice, scabies, and typhoid. She wrote in the Harvard Public Health Alumni Bulletin of measles and whooping cough epidemics that broke out before proper quarantines could be established.
HSPH Professor John E. Gordon, who would go on to chair the Department of Epidemiology, organized units to search for communicable diseases in advance of troops moving into an area, recognizing that until the 20th century, infectious diseases took a greater toll on armies during war than did opposing combatants. Research that Gordon compiled after the war showed that if battle-related mortality were excluded, World War II marked the first conflict in which accidental trauma, such as vehicular accidents, drowning, falls, athletic injuries, and even suicides replaced non-battle-related disease as a major cause of death in the military—part of his keen understanding of the social context of public health trends.
Today’s humanitarian work by HSPH faculty, including those with the Harvard Humanitarian Initiative, mirrors the endeavors undertaken in war-torn areas nearly 70 years ago. At the François-Xavier Bagnoud Center for Health and Human Rights, the mission has evolved and expanded beyond its original focus on HIV/AIDS, said director Jennifer Leaning, to include young people in crushing circumstances—such as girls in poverty-stricken rural India, the Roma in eastern and central Europe, and boys and girls victimized by sex trafficking. “We are focusing on children and adolescents in oppressive, war-torn, grotesque, stigmatized situations around the world.”
Of place and race
Neighborhood effects
If “geography is destiny,” words famously attributed to Napoleon Bonaparte, nowhere is this truer than in the realm of public health. “If there’s one overarching theme, it’s that place matters,” says Ichiro Kawachi, chair of the Department of Social and Behavioral Sciences. “Regardless of who you are as a person, neighborhood makes a big difference in your life chances and your health chances.”

“Regardless of who you are as a person, neighborhood makes a big difference in your life chances and your health chances.” |
One recent strand of investigation took off in the 1970s with the discovery that even unusually high incomes do not protect the health of people living in poor neighborhoods, an insight that emerged from research by Lisa Berkman, now the Thomas Cabot Professor of Public Policy and Epidemiology and director of the Harvard Center for Population and Development Studies. Drawing on a survey of 7,000 adults, Berkman, then a graduate student at the University of California, Berkeley, and her colleagues found a link between income and health—something they had expected. But they were surprised to find that high incomes did not compensate for living in a poor area. On the other hand, the study also found that social connections such as good relationships with friends and family have a protective impact, resulting in longer and healthier lives. Berkman, former chair of the Department of Social and Behavioral Sciences (when it was called the Department of Society, Human Development, and Health), and her successor, Kawachi, established the scholarly framework on social determinants of health at HSPH.
David R. Williams, the Florence Sprague Norman and Laura Smart Norman Professor of Public Health, has explored how socioeconomic status, race, stress, racism, and religious involvement affect physical and mental health. The Everyday Discrimination scale that he developed is currently one of the most widely used instruments in health research to assess perceived discrimination.
The School’s faculty has also shown that just as living in poor, segregated neighborhoods is hazardous to health, so too is living in communities with high levels of income inequality—in part because having substantially less than your neighbors may create significant levels of stress. And HSPH researchers have demonstrated that health is framed not only by a home’s location, but also by what takes place inside that home. Domestic violence—a crime and human rights violation—also raises the risk of asthma, HIV infection, smoking, poor maternal health, and child mortality.
Global nutritionIn the late 1960s, when public health researchers were beginning to understand the significance of diet in resource-limited nations, a seminal report coauthored by three eminent HSPH-affiliated scientists— John E. Gordon, chair of the School’s Epidemiology Department from 1946 to 1958, and nutritionists Nevin S. Scrimshaw, MPH ’59, and Carl E. Taylor, MPH ’51, DPH ’53—exhaustively documented how malnutrition leaves victims more susceptible to infections such as tuberculosis and dysentery, and how infectious disease amplifies the effects of malnutrition. In the mid-1990s, HSPH’s Wafaie Fawzi and colleagues in Tanzania conducted the first clinical trial showing that when HIV-positive women take multivitamins, their chances of miscarriage or of delivering a premature or low-birth-weight baby were reduced by 40 percent. The researchers found that when HIV-infected individuals take daily multivitamin supplements, their disease progressed much more slowly and their chances of dying were greatly reduced. As a result of these findings, nutrition became a core element of HIV/AIDS management with antiretroviral therapy and other interventions. Fawzi’s studies have also shown that during the critical “first 1,000 days”—the duration of pregnancy and the first two years of life—proper nutrition through breastfeeding, a healthy diet, and, when needed, vitamin supplements, dramatically boosts maternal health, decreases premature birth, improves survival and early mental and physical development, and enhances lifelong productivity. Put simply, says Fawzi, proper nutrition early on enhances a person’s prospects in life. “It is simple and inexpensive and doable.”
|
In the late 1990s, Nancy Krieger, professor of social epidemiology, devised a method to portray the link between a community’s health status and its socioeconomic class—a project that arose out of her frustration over the dearth of socioeconomic data in U.S. health records. Krieger statistically linked census tract poverty levels with public health surveillance information, such as all-cause and cause-specific mortality, cancer incidence, and low birth weight. She found that within a federal census tract (an area that usually includes about 4,000 people of similar income and living conditions), the poverty rate corresponds closely with residents’ health status.
Based on this finding, the Public Health Disparities Geocoding Project, launched at HSPH in 2004, has enabled health departments to measure their progress over time, zero in on problems in specific locales, and clarify the links between poverty and disease. In Massachusetts and Rhode Island, for example, Krieger showed that more than half the cases of childhood lead poisoning, sexually transmitted infections, tuberculosis, nonfatal gun-related injuries, and HIV/AIDS deaths among the poorest residents would not have occurred if their risk had been the same as that of people living in the wealthiest enclaves. The geocoding method has been adopted in the U.S. and around the world by researchers and health departments, as well as by the National Cancer Institute.
Healthy growth of people and societies
The measure of a healthy life
“Your child is in the 80th percentile for height and 75th for weight.”
Nearly every parent of an infant or young child in the U.S. and many other parts of the world has heard words similar to those at his or her child’s well-baby visits and annual physicals. But few know the genesis of the charts that doctors use to assess their children’s progress toward normal health milestones—a 1930s project undertaken at Harvard School of Public Health.
The brainchild of pediatrician-researcher Harold Coe Stuart, the Longitudinal Studies of Child Health and Development marked a new approach to pediatric public health. It was concerned with the manifestations of health, not simply sickness, and it replaced a focus on individual care with ongoing developmental research. To this end, Stuart—who headed the School’s Department of Child Hygiene, later known as the Department of Maternal and Child Health—followed a group of 324 children in Boston’s predominantly Irish middle-class Roxbury neighborhood from before birth through adulthood, starting in 1930. The project was holistic and intensely cross-disciplinary—involving social workers, public health nurses, anthropologists, dentists, psychologists, psychiatrists, and pediatricians— a reflection of Stuart’s conviction that children’s health involved the interplay of physical, emotional, social, and cultural factors.
No comprehensive study of normal child growth had ever taken place before. “Pediatricians interested in research have been so preoccupied with the study of disease that they have not contributed as much as might have been anticipated to studies of normal development,” Stuart wrote. “It is surprising how little is really known about the effects of disease on growth, in view of the attention given to sick children.” He advocated that physicians, school health programs, and parents take regular measurements of a child’s height, weight, chest circumference, hip-width, and girth, stressing that diversion from a normal growth pattern might be a tip-off to underlying disease. And presaging more recent social trends, Stuart interviewed fathers and encouraged them to be part of the child’s upbringing.
Download a PDF of Poverty, disasters & health against all odds here
 — Wafaie Fawzi, chair of the Department of Global Health and Population, and professor of nutrition and of epidemiology
— Wafaie Fawzi, chair of the Department of Global Health and Population, and professor of nutrition and of epidemiology